In This Chapter…
Guidelines for a Successful Therapeutic Relationship With a Client Who Has COD
Techniques for Working With Clients With COD
Overview
Maintaining a therapeutic alliance with clients who have co-occurring disorders (COD) is important—and difficult. The first section of this chapter reviews guidelines for addressing these challenges. It stresses the importance of the counselor’s ability to manage feelings and biases that could arise when working with clients with COD (sometimes called countertransference). Together, clinicians and clients should monitor the client’s disorders by examining the status of each disorder and alerting each other to signs of relapse. The consensus panel recommends that counselors use primarily a supportive, empathic, and culturally appropriate approach when working with clients with COD. With some clients who have COD, it is important to distinguish behaviors and beliefs that are cultural in origin from those indicative of a mental disorder. Finally, counselors should increase structure and support to help their clients with COD make steady progress throughout recovery.
The second part of this chapter describes techniques effective in counseling clients with COD. One is the use of motivational enhancement consistent with the client’s specific stage of recovery. This strategy is helpful even for clients whose mental disorder is severe. Other strategies include contingency management, relapse prevention, and cognitive–behavioral techniques. For clients with functional deficits in areas such as understanding instructions, repetition and skill-building strategies can aid progress. Finally, 12-Step and other dual recovery mutual self-help groups have value as a means of supporting individuals with COD in the abstinent life. Clinicians often play an important role in facilitating the participation of these clients in such groups. This chapter will provide a basic overview of how counselors can apply each of these strategies to their clients who have COD. The material in this chapter is consistent with national or State consensus practice guidelines for COD treatment, and consonant with many of their recommendations.
The purpose of this chapter is to describe for the addiction counselor and other practitioners how these guidelines and techniques, many of which are useful in the treatment of substance abuse or as general treatment principles, can be modified specifically and applied to people with COD. These guidelines and techniques are particularly relevant in working with clients in quadrants II and III. Additionally, this chapter contains Advice to the Counselor boxes to highlight the most immediate practical guidance (for a full listing of these boxes see the table of contents).
Guidelines for a Successful Therapeutic Relationship With a Client Who Has COD
The following section reviews seven guidelines that have been found to be particularly helpful in forming a therapeutic relationship with clients who have COD (see text box below).
Guidelines for Developing Successful Therapeutic Relationships With Clients With COD
- Develop and use a therapeutic alliance to engage the client in treatment
- Maintain a recovery perspective
- Manage countertransference
- Monitor psychiatric symptoms
- Use supportive and empathic counseling
- Employ culturally appropriate methods
- Increase structure and support
Develop and Use a Therapeutic Alliance To Engage the Client in Treatment
General. Research suggests that a therapeutic alliance is “one of the most robust predictors of treatment outcome” in psychotherapy (Najavits et al. 2000, p. 2172). Some studies in the substance abuse treatment field also have found associations between the strength of the therapeutic alliance and counseling effectiveness. One research team found that both clinician and client ratings of the alliance were strong predictors of alcoholic outpatients’ treatment participation in treatment, drinking behavior during treatment, and drinking behavior at a 12-month follow-up, even after controlling for a variety of other sources of variance (Connors et al. 1997). Similarly, Luborsky and colleagues (1985) found that the development of a “helping alliance” was correlated with positive outcomes.
A number of researchers have verified that clients are more responsive when the therapist acts consistently as a nurturing and nonjudgmental ally (Frank and Gunderson 1990; Luborsky et al. 1997; Siris and Docherty 1990; Ziedonis and D’Avanzo 1998). For example, in a study of clients with opioid dependence and psychopathology, Petry and Bickel (1999) found that among clients with moderate to severe psychiatric problems, fewer than 25 percent of those with weak therapeutic alliances completed treatment, while more than 75 percent of those with strong therapeutic alliances completed treatment. In this study, they did not find the strength of the therapeutic alliance to be related to treatment completion among clients with few psychiatric symptoms.
Challenges for the clinician
General. The clinician’s ease in working toward a therapeutic alliance also is affected by his or her comfort level in working with the client. Substance abuse counselors may find some clients with significant mental illnesses or severe substance use disorders to be threatening or unsettling. It is therefore important to recognize certain patterns that invite these feelings and not to let them interfere with the client’s treatment. This discomfort may be due to a lack of experience, training, or mentoring. Likewise, some mental health clinicians may feel uncomfortable or intimidated by clients with substance use disorders. Clinicians who experience difficulty forming a therapeutic alliance with clients with COD are advised to consider whether this is related to the client’s difficulties; to a limitation in the clinician’s own experience and skills; to demographic differences between the clinician and the client in areas such as age, gender, education, race, or ethnicity; or to issues involving countertransference (see the discussion of counter-transference below). A consultation with a supervisor or peer to discuss this issue is important. Often these reactions can be overcome with further experience, training, supervision, and mentoring.
Individuals with COD often experience demoralization and despair because of the complexity of having two problems and the difficulty of achieving treatment success. Inspiring hope often is a necessary precursor for the client to give up short-term relief in exchange for long-term work with some uncertainty as to timeframe and benefit.
Advice to the Counselor: Forming a Therapeutic Alliance
The consensus panel recommends the following approaches for forming a therapeutic alliance with clients with COD:
- Demonstrate an understanding and acceptance of the client.
- Help the client clarify the nature of his difficulty.
- Indicate that you and the client will be working together.
- Communicate to the client that you will be helping her to help herself.
- Express empathy and a willingness to listen to the client’s formulation of the problem.
- Assist the client to solve some external problems directly and immediately.
Challenges in working with clients with serious mental and substance use disorders. Achieving a therapeutic alliance with clients with serious mental illness and substance use disorders can be challenging. According to Ziedonis and D’Avanzo (1998), many people who abuse substances also may have some antisocial traits. Such individuals are “less amenable to psychological and pharmacological interventions and avoid contact with the mental health treatment staff.” Therefore, it is reasonable to conclude that “the dually diagnosed are less likely to develop a positive therapeutic alliance than non–substanceabusing patients with schizophrenia…” (p. 443).
Individuals with both schizophrenia and a substance use disorder may be particularly challenging to treat. These individuals “present and maintain a less involved and more distant stance in relation to the therapist than do non–substance-abusing individuals with schizophrenia” (Ziedonis and D’Avanzo 1998, p. 443). The presence or level of these deficits may vary widely for people living with schizophrenia, and also may vary significantly for that individual within the course of his illness and the course of his lifetime. While “this configuration of interpersonal style suggests that developing a therapeutic alliance can be difficult,” Ziedonis and D’Avanzo insist, “working with the dually diagnosed requires a primary focus on the therapeutic alliance” (Ziedonis and D’Avanzo 1998, p. 444).
For all clients with co-occurring disorders, the therapeutic relationship must build on the capacity that does exist. These clients often need the therapeutic alliance to foster not only their engagement in treatment but as the cornerstone of the entire recovery process. Once established, the therapeutic alliance is rewarding for both client and clinician and facilitates their participation in a full range of therapeutic activities; documentation of these types of interactions provides an advantage in risk management.
Maintain a Recovery Perspective
Varied meanings of “recovery”
The word “recovery” has different meanings in different contexts. Substance abuse treatment clinicians may think of a person who has changed his or her substance abuse behavior as being “in recovery” for the rest of his or her life (although not necessarily in formal treatment forever). Mental health clinicians, on the other hand, may think of recovery as a process in which the client moves toward specific behavioral goals through a series of stages. Recovery is assessed by whether or not these goals are achieved. For persons involved with 12-Step programs, recovery implies not only abstinence from drugs or alcohol but also a commitment to “work the steps,” which includes changing the way they interact with others and taking responsibility for their actions. Consumers with mental disorders may see recovery as the process of reclaiming a meaningful life beyond mental disorder, with symptom control and positive life activity.
While “recovery” has many meanings, generally, it is recognized that recovery does not refer solely to a change in substance use, but also to a change in an unhealthy way of living. Markers such as improved health, better ability to care for oneself and others, a higher degree of independence, and enhanced self-worth are all indicators of progress in the recovery process.
Implications of the recovery perspective
The recovery perspective as developed in the substance abuse field has two main features: (1) It acknowledges that recovery is a long-term process of internal change, and (2) it recognizes that these internal changes proceed through various stages (see De Leon 1996 and Prochaska et al. 1992 for a detailed description).
The recovery perspective generates at least two main principles for practice:
- Develop a treatment plan that provides for continuity of care over time. In preparing this plan, the clinician should recognize that treatment may occur in different settings over time (e.g., residential, outpatient) and that much of the recovery process is client-driven and occurs typically outside of or following professional treatment (e.g., through participation in mutual self-help groups) and the counselor should reinforce long-term participation in these constantly available settings.
- Devise treatment interventions that are specific to the tasks and challenges faced at each stage of the COD recovery process. The use of treatment interventions that are specific to the tasks and challenges faced at each stage of the COD recovery process enables the clinician (whether within the substance abuse or mental health treatment system) to use sensible stepwise approaches in developing and using treatment protocols. In addition, markers that are unique to individuals— such as those related to their cultural, social, or spiritual context—should be considered. It is therefore important to engage the client in defining markers of progress that are meaningful to him and to each stage of recovery.
Advice to the Counselor: Maintaining a Recovery Perspective
The consensus panel recommends the following approaches for maintaining a recovery perspective with clients who have COD:
- Assess the client’s stage of change (see section on Motivational Enhancement below).
- Ensure that the treatment stage (or treatment expectations) is (are) consistent with the client’s stage of change.
- Use client empowerment as part of the motivation for change.
- Foster continuous support.
- Provide continuity of treatment.
- Recognize that recovery is a long-term process and that even small gains by the client should be supported and applauded.
Stages of change and stages of treatment
Working within the recovery perspective requires a thorough understanding of the interrelationship between stages of change (see De Leon 1996 and Prochaska et al. 1992) and stages of treatment (see section on motivational enhancement below for a description of the stages of change; see also TIP 35, Enhancing Motivation for Change in Substance Abuse Treatment [Center for Substance Abuse Treatment (CSAT) 1999b]). De Leon has developed a measure of motivation for change and readiness for treatment— The Circumstances, Motivation and Readiness Scales—and provided scores for samples of persons with COD (De Leon et al. 2000a). De Leon has demonstrated the relationship between these scales and retention in treatment for general substance abuse treatment populations and programs (De Leon 1996). It is important that the expectation for the client’s progress through treatment stages (e.g., outreach, stabilization, early-middle-late primary treatment, continuing care, and long-term care/cycles into and out of treatment) be consistent with the client’s stage of change.
Client empowerment and responsibility
The recovery perspective also emphasizes the empowerment and responsibility of the client and the client’s network of family and significant others. As observed by the American Association of Community Psychiatrists (AACP), the strong client empowerment movement within the mental health field is a cornerstone for recovery:
Pessimistic attitudes about people with COD represent major barriers to successful system change and to effective treatment interventions … recovery is defined as a process by which a person with persistent, possibly disabling disorders, recovers self-esteem, self-worth, pride, dignity, and meaning, through increasing his or her ability to maintain stabilization of the disorders and maximizing functioning within the constraints of the disorders. As a general principle, every person, regardless of the severity and disability associated with each disorder, is entitled to experience the promise and hope of dual recovery, and is considered to have the potential to achieve dual recovery (AACP 2000b).
Continuous support
Another implication of the recovery perspective is the need for continuing support for recovery. This means the provider encourages clients to build a support network that offers respect, acceptance, and appreciation. For example, an important element of long-term participation in Alcoholics Anonymous (AA) is the offering of a place of belonging or a “home.” AA accomplishes this supportive environment without producing overdependence because the client is expected to contribute, as well as receive, support.
Continuity of treatment
An emphasis on continuity of treatment also flows from a recovery perspective. Continuity of treatment implies that the services provided by the program are constant, and a client might remain a consumer of substance abuse or mental health services indefinitely. Treatment continuity for individuals with COD begins with proper and thorough identification, assessment, and diagnosis. It includes easy and early access to the appropriate service providers “…through multiple episodes of acute and subacute treatment … independent of any particular setting or locus of care” (AACP 2000b).
Manage Countertransference
Though somewhat dated and infrequently used in the COD literature, the concept of “countertransference” is useful for understanding how the clinician’s past experience can influence current attitudes toward a particular client.
“Transference” describes the process whereby clients project attitudes, feelings, reactions, and images from the past onto the clinician. For example, the client may regard the clinician as an “authoritative father,” “know-it-all older brother,” or “interfering mother.”
Once considered a technical error, countertransference now is understood to be part of the treatment experience for the clinician. Particularly when working with multiple and
complicated problems, clinicians are vulnerable to the same feelings of pessimism, despair, anger, and the desire to abandon treatment as the client. Inexperienced clinicians often are confused and ashamed when faced with feelings of anger and resentment that can result from situations where there is a relative absence of gratification from working with clients with these disorders (Cramer 2002). Less experienced practitioners may have more difficulty identifying countertransference, accessing feelings evoked by interactions with a client, naming them, and working to keep these feelings from interfering with the counseling relationship.
Advice to the Counselor: Managing Countertransference
The consensus panel recommends the following approach for managing countertransference with clients who have COD:
- The clinician should be aware of strong personal reac-tions and biases toward the client.
- The clinician should obtain further supervision where countertransference is suspected and may be interfering with counseling.
- Clinicians should have formal and periodic clinical supervision to discuss countertransference issues with their supervisors and the opportunity to discuss these issues at clinical team meetings.
Both substance use disorders and mental disorders are illnesses that are stigmatized by the general public. These same attitudes can be present among clinicians. Mental health clinicians who usually do not treat persons with substance abuse issues may not have worked out their own response to the disorder, which can influence their interactions with the client. Similarly, substance abuse treatment clinicians may not be aware of their own reactions to persons with specific mental disorders and may have difficulty preventing these reactions from influencing treatment. The clinician’s negative attitudes or beliefs may be communicated, directly or subtly, to the client. For example: “I was depressed too, but I never took medications for it—I just worked the steps and got over it. So why should this guy need medication?”
Such feelings often are related to burnout and are exacerbated by the long time required to see progress in many clients with COD. For example, one study found that therapists’ attitudes toward their substance abuse clients tended to become more negative over time, though the increasing negativity was found to be less extreme for substance abuse counselors without graduate degrees who used the 12 steps to inform their counseling approach than for psychotherapists with graduate training who participated in the study (Najavits et al. 1995). (For a full discussion of countertransference in substance abuse treatment see Powell and Brodsky 1993.)
Cultural issues also may arouse strong and often unspoken feelings and, therefore, generate transference and countertransference. Although counselors working with clients in their area of expertise may be familiar with countertransference issues, working with an unfamiliar population will introduce different kinds and combinations of feelings.
The clinician is advised to understand and be familiar with some of the issues related to countertransference and strategies to manage it. Such countertransference issues are particularly
important when working with persons with COD because many people with substance abuse and mental disorders may evoke strong feelings in the clinician that could become barriers to treatment if the provider allows them to interfere. The clinician may feel angry, used, overwhelmed, confused, anxious, uncertain how to proceed with a case, or just worn out.
Monitor Psychiatric Symptoms
In working with clients who have COD, especially those requiring medications or who also are receiving therapy from a mental health services provider, it is especially important for the substance abuse counselor to participate in the development of the treatment plan and to monitor psychiatric symptoms. At a minimum, the clinician should be knowledgeable about the overall treatment plan to permit reinforcement of the mental health part of the plan as well as the part specific to recovery from addiction.
It is equally important that the client participate in the development of the treatment plan. For example, for a client who has both bipolar disorder and alcoholism, and who is receiving treatment at both a substance abuse treatment agency and a local mental health center, the treatment plan might include individual substance abuse treatment counseling, medication management, and group therapy. In another example, the substance abuse treatment clinician may assist in medication monitoring of a person taking lithium. The clinician can ask such questions as, “How are your meds doing? Are you remembering to take them? Are you having any problems with them? Do you need to check in with the prescribing doctor?” It also is prudent to ask the client to bring in all medications and ask the client how he is taking them, when, how much, and if medication is helping and how. Clinicians should help educate clients about the effects of medication, teach clients to monitor themselves (if possible), and consult with clients’ physicians whenever appropriate.
Advice to the Counselor: Monitoring Psychiatric Symptoms
The consensus panel recommends the following approaches for monitoring psychiatric symptoms with clients with COD:
- Obtain a mental status examination to evaluate the client’s overall mental health and danger profile. Ask questions about the client’s symptoms and use of medication and look for signs of the mental disorder regularly.
- Keep track of changes in symptoms.
- Ask the client directly and regularly about the extent of his or her depression and any associated suicidal thoughts.
Status of symptoms
Substance abuse counselors need to have a method by which to monitor changes in severity and number of symptoms over time. For example, most clients present for substance abuse treatment with some degree of anxiety or depressive symptoms. As discussed in chapters 2 and 4, these symptoms are referred to as substance induced if caused by substances and resolved within 30 days of abstinence. Substance-induced symptoms tend to follow the “teeter totter” principle of “what goes up, must come down,” and vice versa—so that after a run of amphetamine or cocaine the individual will appear fatigued and depressed, while after using depressants such as alcohol or opioids, the individual more likely will appear agitated and anxious. These “teeter totter” symptoms are substance withdrawal effects and usually are seen for days or weeks. They may be followed by a substance-related depression (which can be seen as a neurotransmitter depletion state), which should begin to improve within a few weeks. If depressive or other symptoms persist, then a co-occurring (additional) mental disorder is likely, and the differential diagnostic process ensues. These symptoms may be appropriate target symptoms for establishing a diagnosis or determining treatment choices (medication, therapy, etc.). Clients using methamphetamines may present with psychotic symptoms that require medications.
A number of different tools are available to substance abuse treatment providers to help monitor psychiatric symptoms. Some tools are simply questions and require no formal instrument. For example, to gauge the status of depression quickly, ask the client: “On a scale of 0 to 10, how depressed are you? (0 is your best day, 10 is your worst).” This simple scale, used from session to session, can provide much useful information. Adherence to prescribed medication also should be monitored by asking the client regularly for information about its use and effect.
To identify changes, it is important to track symptoms that the client mentions at the onset of treatment from week to week. The clinician should keep track of any suggestions made to the client to alleviate symptoms to determine whether the client followed through, and if so, with what result. For example: “Last week you mentioned low appetite, sleeplessness, and a sense of hopelessness. Are these symptoms better or worse now?”
Potential for harm to self or others
Blumenthal (1988) has written an important paper on suicide and the risk for suicide in clients with COD. The following is derived largely from her writing.
Suicidality is a major concern for many clients with COD. Persons with mental disorders are at 10 times greater risk for suicide than the general population, and the risk for suicidal behavior and suicide is increased with almost every major mental disorder. Of adults who commit suicide, 90 percent have a mental disorder, most frequently a major affective illness or posttraumatic stress disorder (PTSD). Alcohol and substance abuse often are associated with suicides and also represent major risk factors. Clients with COD—especially those with affective disorders—have two of the highest risk factors for suicide.
For clients who mention or appear to be experiencing depression or sadness, it is always important to explore the extent to which suicidal thinking is present. Similarly, a client who reports that he or she is thinking of doing harm to someone else should be monitored closely. The clinician always should ask explicitly about suicide or the intention to do harm to someone else when the client assessment indicates that either is an issue.
In addition to asking the client about suicidal thoughts and plans as a routine part of every session with a suicidal or depressed person, Blumenthal stresses that the clinician should immediately follow up appointments missed by an acutely suicidal person. Management of the suicidal client requires securing an appropriate mental health professional for the client and having the client monitored closely by that mental health professional. The counselor also should have 24-hour coverage available, such as a hotline for the client to call for help during off hours. However, there are effective ways of managing individuals who have suicidal thoughts but no immediate plan, and are willing and able to contact the counselor in the event these thoughts become too strong, prior to action. See the more extensive discussion of suicidality in chapter 8 and in appendix D of this TIP. Screening for suicide risk is discussed in chapter 4.
Use Supportive and Empathic Counseling
Definition and importance
A supportive and empathic counseling style is one of the keys to establishing an effective therapeutic alliance. According to Ormont, empathy is the ability to “experience another person’s feeling or attitude while still holding on to our own attitude and outlook”; it is the foundation adults use for relating to and interacting with other adults (Ormont 1999, p. 145). The clinician’s empathy enables clients to begin to recognize and own their feelings, an essential step toward managing them and learning to empathize with the feelings of others.
However, this type of counseling must be used consistently over time to keep the alliance intact. This caveat often is critical for clients with COD, who usually have lower motivation to address either their mental or substance abuse problems, have greater difficulty understanding and relating to other people, and need even more understanding and support to make a major lifestyle change such as adopting abstinence. Support and empathy on the clinician’s part can help maintain the therapeutic alliance, increase client motivation, assist with medication adherence, model behavior that can help the client build more productive relationships, and support the client as he or she makes a major life transition.
Using an Empathic Style
Empathy is a key skill for the counselor, without which little could be accomplished. The practice of empathy “requires sharp attention to each new client statement, and a continual generation of hypotheses as to the underlying meaning” (Miller and Rollnick 1991, p. 26). An empathic style
- Communicates respect for and acceptance of clients and their feelings
- Encourages a nonjudgmental, collaborative relationship
- Allows the clinician to be a supportive and knowledgeable consultant
- Compliments and reinforces the client whenever possible
- Listens rather than tells
- Gently persuades, with the understanding that the decision to change is the client’s
- Provides support throughout the recovery process
(See also TIP 35, Enhancing Motivation for Change in Substance Abuse Treatment [CSAT 1999b], p. 41.)
Confrontation and empathy
The overall utility of confrontational techniques is well accepted in the substance abuse literature. It is used widely in substance abuse treatment programs, including those surveyed in the Drug Abuse Treatment Outcomes Study in which the effectiveness of such programs was demonstrated. Confrontation is a form of interpersonal exchange in which individuals present to each other their observations of, and reactions to, behaviors and attitudes that are matters of concern and should change (De Leon 2000b).
In substance abuse treatment counseling, some tension always is felt between being empathic and supportive, and having to handle minimization, evasion, dishonesty, and denial. However, a counselor can be empathic and firm at the same time. This is especially true when working with clients with COD. The heart of confrontation is not the aggressive breaking down of the client and his or her defenses, but feedback on behavior and the compelling appeal to the client for personal honesty, truthfulness in interacting with others, and responsible behavior. A straightforward and factual presentation of conflicting material or of problematic behavior in an inquisitive and caring manner can be both “confrontative” and caring. The ability to do this well and with balance often is critical in maintaining the therapeutic alliance with a client who has COD. Chapter 6 includes a more complete discussion of confrontation including a definition, description of its application, and suggested modifications for using this technique with clients who have COD.
Employ Culturally Appropriate Methods
Understanding the client’s cultural background
It is well known that population shifts are resulting in increasing numbers of minority racial and ethnic groups in the United States. Each geographic area has its own cultural mix, and providers are advised to learn as much as possible about the cultures represented in their treatment populations. Of particular importance are the backgrounds of those served, conventions of interpersonal communication, understanding of healing, views of mental disorder, and perception of substance abuse.
To work effectively with persons of various cultural groups, the provider should learn as much as possible about characteristics of the cultural group such as communication style, interpersonal interactions, and expectations of family. For example, some cultures may tend to somaticize symptoms of mental disorders, and clients from such groups may expect the clinician to offer relief for physical complaints. The same client may be offended by too many probing, personal questions early in treatment and never return. Similarly, understanding the client’s role in the family and its cultural significance always is important (e.g., expectations of the oldest son, a daughter’s responsibilities to her parents, grandmother as matriarch).
At the same time, the clinician should not make assumptions about any client based on his or her perception of the client’s culture. The level of acculturation and the specific experiences of an individual may result in that person identifying with the dominant culture, or even other cultures. For example, a person from India adopted by American parents at an early age may know little about the cultural practices in his birth country. For such clients, it is still important to recognize the birth country and discover what this association means to the client; however, it may exert little influence on his beliefs and practices. For more detailed information about cultural issues in substance abuse treatment, see the forthcoming TIP Improving Cultural Competence in Substance Abuse Treatment (CSAT in development a).
Clients’ perceptions of substance abuse, mental disorders, and healing
Clients may have culturally driven concepts of what it means to abuse substances or to have a mental disorder, what causes these disorders, and how they may be “cured.” Clinicians are encouraged to explore these concepts with people who are familiar with the cultures represented in their client population. Counselors should be alert to differences in how their role and the healing process are perceived by persons who are of cultures other than their own. Wherever appropriate, familiar healing practices meaningful to these clients should be integrated into treatment. An example would be the use of acupuncture to calm a Chinese client or help control cravings, or the use of traditional herbal tobacco with some American Indians to establish rapport and aid emotional balance.
Advice to the Counselor: Using Culturally Appropriate Methods
The consensus panel recommends the following approach for using culturally appropriate treatment methods with clients with COD:
- • Take cultural context, background, and experiences into account in the evaluation, diagnosis, and treatment of clients from various groups, cultures, or countries.
- • Recognize the importance of culture and language, acknowledging the cultural strengths of a people.
- • Adapt services to meet the unique needs and value systems of persons in all groups.
- • Expand and update [the provider’s/system’s] cultural knowledge.
- • Work on stigma reduction with a culturally sensitive approach.
Source: Center for Mental Health Services 2001.
Cultural perceptions and diagnosis
It is important to be aware of cultural and ethnic bias in diagnosis. For example, in the past some African Americans were stereotyped as having paranoid personality disorders, while women have been diagnosed frequently as being histrionic. American Indians with spiritual visions have been misdiagnosed as delusional or as having borderline or schizotypal personality disorders. Some clinicians would be likely to over diagnose obsessive-compulsive disorder among Germans or histrionic disorder in Hispanic/Latino populations. The diagnostic criteria should be tempered by sensitivity to cultural differences in behavior and emotional expression and by an awareness of the clinician’s own biases and stereotyping.
Cultural differences and treatment: Empirical evidence on effectiveness
Studies related to cultural differences and treatment issues among clients with COD are scarce. However, one study that compared nonwhite and white clients with COD who were treated in mental health settings suggests issues that deserve providers’ attention. Researchers found that African-American, Asian-American, and Hispanic/Latino clients tended to self-report a lower level of functioning and to be “viewed by clinical staff as suffering from more severe and persistent symptomatology and as having lower psychosocial functioning.” Researchers noted “this was due in part to the chronicity of their mental disorders and persistent substance abuse, but also was magnified by cross-cultural misperceptions; for example, system bias, countertransference, or inadequate support systems” (Jerrell andWilson 1997, p. 138).
The study also found that nonwhite clients tended to have fewer community resources available to them than white clients, and that clinicians had more difficulty connecting them with needed services. For example, staff members experienced “extraordinary difficulties in identifying willing and suitable sponsors for the young ethnic clients” in 12-Step programs (Jerrell and Wilson 1997, p. 138). To address such issues, researchers stressed the importance of developing cultural competence in staff, giving extra attention to the needs of such clients, and engaging in “more active advocacy for needed, culturally relevant services” (Jerrell and Wilson 1997, p. 139).
Increase Structure and Support
To assist clients with COD, counselors should provide an optimal amount of structure for the individual. Free time is both a trigger for substance use cravings and a negative influence for many individuals with mental disorders; therefore it is a particular issue for clients with COD. Strategies for managing free time include structuring one’s day to have meaningful activities and to avoid activities that will be risky. Clinicians often help clients to plan their time (especially weekends). Creating new pleasurable activities can both help depression and help derive “highs” from sources other than substance use. Other important activities to include are working on vocational and relationship issues.
In addition to structure, it is also important that the daily activities contain opportunities for receiving support and encouragement. Counselors should work with clients to create a healthy support system of friends, family, and activities. Increasing support, time organization, and structured activities are strategies in cognitive–behavioral therapies (see section below) for both mental disorders and substance abuse treatment.
Techniques for Working With Clients With COD
The following section reviews techniques, mainly from the substance abuse field, that have been found to be particularly helpful in the treatment of clients with substance abuse and that are being adapted for work with clients with COD (see text box below).
Key Techniques for Working With Clients Who Have COD
- Provide motivational enhancement consistent with the client’s specific stage of change.
- Design contingency management techniques to address specific target behaviors.
- Use cognitive–behavioral therapeutic techniques.
- Use relapse prevention techniques.
- Use repetition and skills-building to address deficits in functioning.
- Facilitate client participation in mutual self-help groups.
Provide Motivational Enhancement Consistent With the Client’s Specific Stage of Change
Definition and description
Motivational Interviewing (MI) is a “client-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence” (Miller and Rollnick 2002, p. 25). MI has proven effective in helping clients clarify goals and make commitment to change (CSAT 1999b; Miller 1996; Miller and Rollnick 2002; Rollnick and Miller 1995). This approach shows so much promise that it is one of the first two psychosocial treatments being sponsored in multisite trials in the National Institute on Drug Abuse (NIDA) Clinical Trials Network program.
As Miller and Rollnick have pointed out, MI is “a way of being with a client, not just a set of techniques for doing counseling” (Miller and Rollnick 1991, p. 62). This approach involves accepting a client’s level of motivation, whatever it is, as the only possible starting point for change. For example, if a client says she has no interest in changing her drinking amounts or frequency, but only is interested in complying with the interview to be eligible for something else (such as the right to return to work or a housing voucher),the clinician would avoid argumentation or confrontation in favor of establishing a positive rapport with the client—even remarking on the positive aspect of the client wishing to return to work or taking care of herself by obtaining housing. The clinician would seek to probe the areas in which the client does have motivation to change. The clinician is interested in eventually having an impact on the client’s drinking or drug use, but the strategy is to get to that point by working with available openings.
A variety of adaptations of MI have emerged. Examples include brief negotiation, motivational consulting, and motivational enhancement therapy (MET). MET combines the clinical style associated with MI with systematic feedback of assessment results in the hope of producing rapid, internally motivated change. For more information, see the Project MATCH Motivational Enhancement Therapy Manual (National Institute on Alcohol Abuse and Alcoholism 1994). Rollnick and other practitioners of MI find that the many variants differ widely in their reliance on the key principles and elements of MI (Miller and Rollnick 2002).
Guiding principles of motivational interviewing
The four principles outlined below guide the practice of MI (see text box p. 114). In this section, each principle is summarized. For each principle, some of the related strategies that practitioners use when applying this principle to client interactions are highlighted.
1. Expressing empathy
Miller and Rollnick state that “an empathic counseling style is one fundamental and defining characteristic of motivational interviewing” (Miller and Rollnick 2002, p. 37). The counselor refrains from judging the client; instead, through respectful, reflective listening, the counselor projects an attitude of acceptance. This acceptance of the person’s perspectives does not imply agreement. It “does not prohibit the counselor from differing with the client’s views and expressing that divergence” (Miller and Rollnick 2002, p. 37). It simply accepts the individual’s ambivalence to change as normal and expected behavior in the human family. Practitioners find that projecting acceptance rather than censure helps free the client to change (Miller and Rollnick 2002).
2. Developing discrepancies
While recognizing the client’s ambivalence to change as normal, the counselor is not neutral or ambivalent about the need for change. The counselor advances the cause of change not by insisting on it, but by helping the client perceive the discrepancy between the current situation and the client’s personal goals (such as a supportive family, successful employment, and good health). The task of the counselor is to call attention to this discrepancy between “the present state of affairs and how one wants it to be,” making it even more significant and larger in the client’s eyes. The client is therefore more likely to change, because he sees that the current behavior is impeding progress to his goals—not the counselor’s (Miller and Rollnick 2002, p. 39).
3. Rolling with resistance
Practitioners believe that “the least desirable situation, from the standpoint of evoking change, is for the counselor to advocate for change while the client argues against it” (Miller and Rollnick 2002, p. 39). The desired situation is for clients themselves to make the argument for change. Therefore, when resistance is encountered, the counselor does not oppose it outright. Instead, the counselor offers new information and alternative perspectives, giving the client respectful permission to “take what you want and leave the rest” (Miller and Rollnick 2002, p. 40).
The counselor’s response to resistance can defuse or inflame it. Miller and Rollnick describe a number of techniques the skillful clinician can use when resistance is encountered.
For example, the counselor may use various forms of reflection, shift the focus of discussion, reframe the client’s observation, or emphasize the client’s personal choice or control. While description of these and other specific techniques for “rolling with resistance” is beyond the scope of this TIP, the reader is referred to chapter 8 of Miller and Rollnick 2002, “Responding to Resistance” (pp. 98–110).
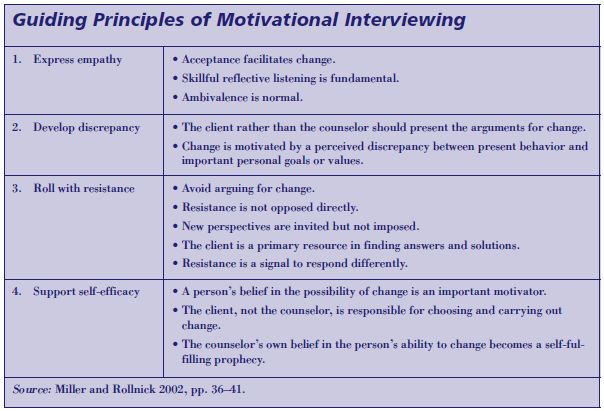
4. Supporting self-efficacy
The final principle of Motivational Interviewing recognizes that an individual must believe he or she actually can make a change before attempting to do so. Therefore, the counselor offers support for the change and communicates to the client a strong sense that change is possible. Self-efficacy also can be enhanced through the use of peer role models, as well as by pointing out past and present evidence of the client’s capacity for change.
One way practitioners put this principle into action is by evoking “confidence talk” in which the client is invited to share “ideas, experiences, and perceptions that are consistent with ability to change” (Miller and Rollnick 2002, p. 113). This could involve reviewing past successes, discussing specific steps for making change happen, identifying personal strengths, and acknowledging sources of support.
“Change talk”
Clients’ positive remarks about change, or “change talk,” are the opposite of resistance. The counselor responds to any expression of desire to change with interest and encourages the client to elaborate on the statement. For example in a person with combined alcohol dependence and PTSD, the clinician might ask, “What are some other reasons why you might want to make a change?” (Miller and Rollnick 2002, p. 87). The counselor also can use reflective listening to clarify the client’s meaning and explore what is being said. It is important, however, to do this in a way that does not appear to be taking a side in the argument. This sometimes results in resistance and the client may begin to argue with the counselor instead of continuing to think about change.
“Decisional balance”
Practitioners of MI have coined the term “decisional balance” to describe a way of looking at ambivalence. Picture a seesaw, with the costs of the status quo and the benefits of change on one side, and the costs of change and the benefits of the status quo on the other (Miller and Rollnick 2002). The counselor’s role is to explore the costs and benefits of substance use with the aim of tipping the balance toward change. That change will be stronger and more likely to endure if it is owned by the client’s perception that the benefits of change are greater than the costs.
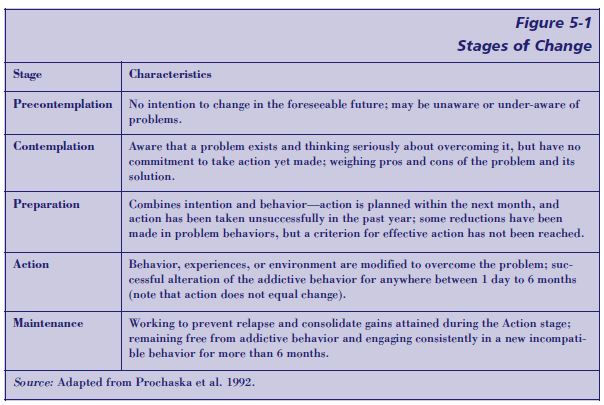
Matching motivational strategies to the client’s stage of change
The motivational strategies selected should be consistent with the client’s stage of change (summarized in Figure 5-1, p. 116). Clients could be at one stage of recovery or change for the mental disorder and another for the substance use disorder; to complicate things further, a client may be at one stage of change for one substance and another stage of change for another substance. For example, a client with combined alcohol and cocaine dependence with co-occurring panic disorder may be in the contemplation stage (i.e., aware that a problem exists and considering overcoming it, but not committed to taking action) in regard to alcohol, precontemplation (i.e., unaware that a problem exists, with no intention of changing behavior) in regard to cocaine, and action (i.e., actively modifying behavior, experiences, or environment to overcome the problem) for the panic disorder.
In each case, the clinician examines the internal and external leverage available to move the client toward healthy change. For example, a client may want to talk about her marriage, but not about the substance abuse problem. The clinician can use this as an opening; the marriage doubtless will be affected by the substance abuse, and the motivation to improve the marriage may lead to a focus on substance abuse. Evaluating a client’s motivational state necessarily is an ongoing process. It should be recognized that court mandates, rules for clients engaged in group therapy, the treatment agency’s operating restrictions, or other factors may place some barriers on how this strategy is implemented in particular situations.
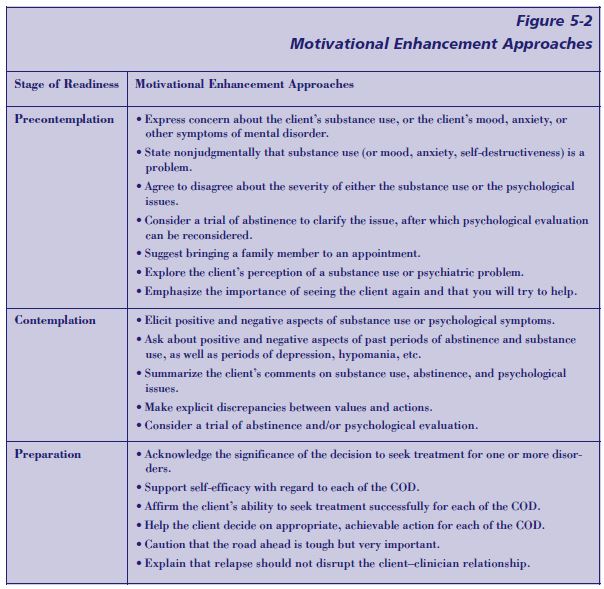
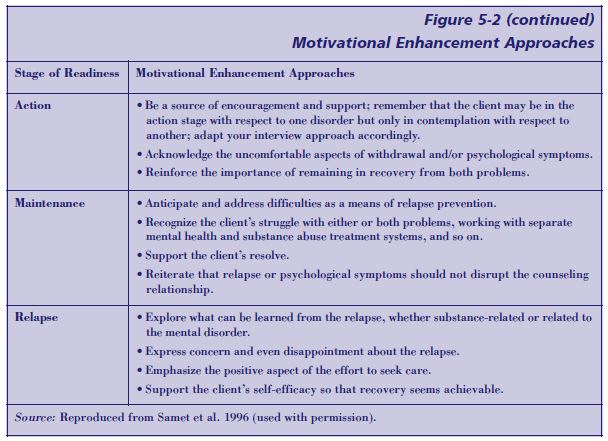
Figure 5-2 (pp. 117–118) illustrates approaches that a clinician might use at different stages of readiness to change to apply MI techniques when working with a substance abuse client showing evidence of COD. For a thorough discussion of MI and the stages of change, the reader is referred to Miller and Rollnick 2002 (pp. 201–216).
Although MI is a well-accepted and commonly used strategy in the substance abuse treatment field, the issue of when it is appropriate to avoid or postpone addressing the client’s substance use is the subject of some debate. MI does make a distinction between agreeing with a client’s denial system (which is counterproductive) and sidestepping it in order to make some progress. As shown above, these motivational strategies are employed to help both clinician and client work together toward the common goal of helping the client. With practice and experience, the clinician will come to recognize when to sidestep disagreements and pursue MI and when to move forward with traditional methods with clients who are motivated sufficiently and ready for change. The details of these strategies and techniques are presented in TIP 35 (CSAT 1999b) and in Miller and Rollnick 2002.
Motivational interviewing and co-occurring disorders
Approaches based on MI have been adapted for people with COD with some initial evidence of efficacy for improved treatment engagement. In a sample of 100 inpatient clients with COD from a large university hospital, Daley and Zuckoff (1998, p. 472) found that with only one “motivational therapy” session prior to hospital discharge, “…the show rate for the initial outpatient appointment almost doubled, increasing from 35 percent to 67 percent.” In this study MI approaches were modified to focus on contrasting the goals and methods of hospital and outpatient treatment. Also, the client was invited to consider the advantages and challenges of continuing in outpatient treatment. Daley and Zuckoff’s results are relevant for people in most quadrants (see chapters 2 and 3), as the majority of their clientele are described as “public sector clients who have mood, anxiety, personality, or psychotic disorders combined with alcohol, cocaine, heroin, sedative hypnotic, cannabis, or polysubstance use disorders.”
Swanson and colleagues (1999) modified MI techniques by increasing the amount of discussion of the client’s perception of the problem and his understanding of his clinical condition. Of the 121 study participants who were selected from psychiatric inpatients at two inner-city hospitals, 93 had concomitant substance use disorders. Participants were assigned randomly to either standard treatment or standard treatment with the addition of a motivational interview. The MI focused on exploring the clients’ commitment to treatment, plans for continuing care, and understanding of their role in their own recovery.
Essentially, the therapists were attempting to elicit a motivational statement that indicated the clients’ commitment to treatment. The authors found that, whether considering the entire sample or only those with COD, study participants who received the MI were significantly more likely to attend an initial outpatient treatment session.
Motivational strategies have been shown to be helpful with persons who have serious mental disorders. Most programs designed for persons with such disorders recognize “that the majority of psychiatric clients have little readiness for abstinence-oriented substance use disorder (SUD) treatments;” therefore, they “incorporate motivational interventions designed to help clients who either do not recognize their SUD or do not desire substance abuse treatment to become ready for more definitive interventions aimed at abstinence” (Drake and Mueser 2000).
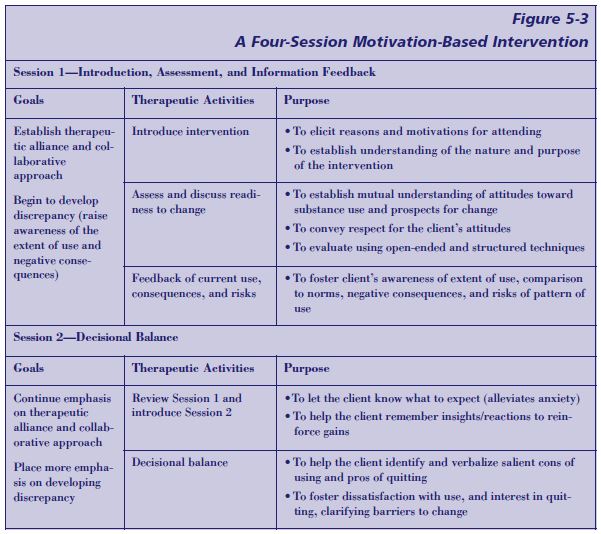
A four-session intervention has been developed specifically to enhance readiness for change and treatment engagement of persons with schizophrenia who also abuse alcohol and other substances (Carey et al. 2001). This intervention is summarized in Figure 5-3 (p. 119). In a pilot study of the intervention, 92 percent of the 22 participants completed the series of sessions, all of whom reported that intervention was both positive and helpful. A range of motivational variables showed post-intervention improvements in recognition of substance use problems and greater treatment engagement, confirmed by independent clinician ratings. Those who began the intervention with low problem recognition made gains in that area; those who began with greater problem recognition made gains in the frequency of use and/or involvement in treatment. Although these data are preliminary, the technique is well articulated. It shows promise and warrants further research, including efforts to determine its efficacy among clients with COD who have mental disorders other than schizophrenia.
It should be noted, however, that assessment of readiness to change could differ markedly between the client and the clinician. Addington et al. (1999) found little agreement between self-report of stage of readiness to change and the assessment of stage of readiness determined by interviewers for their 39 outpatients with diagnoses of both schizophrenia and a substance use disorder. In view of these observations, clinicians should be careful to establish a mutual agreement on the issue of readiness to change with their clients.
Applying the motivational interviewing approach to clients with COD
To date, motivational interviewing strategies have been applied successfully to the treatment of clients with COD, especially in
- Assessing the client’s perception of the problem
- Exploring the client’s understanding of his or her clinical condition
- Examining the client’s desire for continued treatment
- Ensuring client attendance at initial sessions
- Expanding the client’s assumption of responsibility for change Future directions include
- Further modification of MI protocols to make them more suitable for clients with COD, particularly those with serious mental disorders
- Tailoring and combining MI techniques with other treatments to solve the problems (e.g., engagement, retention, etc.) of all treatment modalities
See the text box below for a case study applying MET.
Design Contingency Management Techniques To Address Specific Target Behaviors
Description
Contingency Management (CM) maintains that the form or frequency of behavior can be altered through a planned and organized system of positive and negative consequences. CM assumes that neurobiological and environmental factors influence substance use behaviors and that the consistent application of reinforcing environmental consequences can change these behaviors. CM principles for substance abuse treatment have been structured around four central principles (Higgins and Petry 1999):
- The clinician arranges for regular drug testing to ensure the client’s use of the targeted substance is detected readily.
- The clinician provides positive reinforcement when abstinence is demonstrated. These positive reinforcers are agreed on mutually.
- The clinician withholds the designated incentives from the individual when the substance is detected.
- The clinician helps the client establish alternate and healthier activities.
CM techniques are best applied to specific targeted behaviors such as
- Drug abstinence
- Clinic attendance and group participation
- Medication adherence
- Following treatment plan
- Attaining particular goals
The clinician may use a variety of CM techniques or reinforcers. The most common are
- Cash
- Vouchers
- Prizes
- Retail items
- Privileges
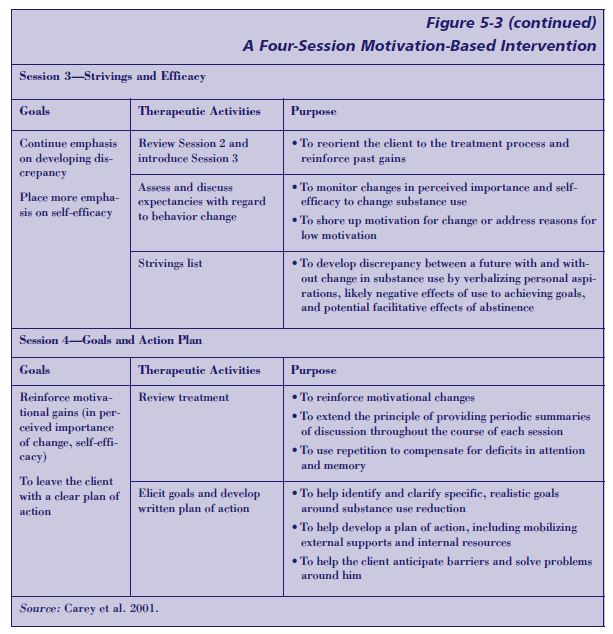
Figure 5-4 contains a checklist for a clinician designing CM programs. See also p. 124 for a case study applying CM.
Case Study: Using MET With a Client Who Has COD
Gloria M. is a 34-year-old African-American female with a 10-year history of alcohol dependence and 12-year history of bipolar disorder. She has been hospitalized previously both for her mental disorder and for substance abuse treatment. She has been referred to the outpatient substance abuse treatment provider from inpatient substance abuse treatment services after a severe alcohol relapse.
Over the years, she sometimes has denied the seriousness of both her addiction and mental disorders. Currently, she is psychiatrically stable and is prescribed valproic acid to control the bipolar disorder. She has been sober for 1 month.
At her first meeting with Gloria M., the substance abuse treatment counselor senses that she is not sure where to focus her recovery efforts—on her mental disorders or her addiction. Both have led to hospitalization and to many life problems in the past. Using motivational strategies, the counselor first attempts to find out Gloria M.’s own evaluation of the severity of each disorder and its consequences to determine her stage of change in regard to each one.
Gloria M. reveals that while in complete acceptance and an active stage of change around alcohol dependence, she is starting to believe that if she just goes to enough recovery meetings she will not need her bipolar medication. Noting her ambivalence, the counselor gently explores whether medications have been stopped in the past and, if so, what the consequences have been. Gloria M. recalls that she stopped taking medications on at least half a dozen occasions over the last 10 years; usually, this led her to jail, the emergency room, or a period of psychiatric hospitalization. The counselor explores these times, asking: Were you feeling then as you were now—that you could get along? How did that work out? Gloria M. remembers believing that if she attended 12-Step meetings and prayed she would not be sick. In response to the counselor’s questions, she observes, “I guess it hasn’t ever really worked in the past.”
The counselor then works with Gloria M. to identify the best strategies she has used for dual recovery in the past. “Has there been a time you really got stable with both disorders?” Gloria M. recalls a 3-year period between the ages of 25 and 28 when she was stable, even holding a job as a waitress for most of that period. During that time, she recalls, she saw a psychiatrist at a local mental health center, took medications regularly, and attended AA meetings frequently. She recalls her sponsor as being supportive and helpful. The counselor then affirms the importance of this period of success and helps Gloria M. plan ways to use the strategies that have already worked for her to maintain recovery in the present.
Empirical evidence on the effectiveness of contingency management
A substantial empirical base supports CM techniques, which have been applied effectively to a variety of behaviors. CM techniques have demonstrated effectiveness in enhancing retention and confronting drug use (e.g., Higgins 1999; Petry et al. 2000). The techniques have been shown to address use of a variety of specific substances, including opioids (e.g., Higgins et al. 1986; Magura et al. 1998), marijuana (Budney et al. 1991), alcohol (e.g., Petry et al. 2000), and a variety of other drugs including cocaine (Budney and Higgins 1998). However, CM techniques have not been implemented in community-based settings until recently. The use of vouchers and other reinforcers has considerable empirical support (e.g., Higgins 1999; Silverman et al. 2001), but little evidence is apparent for the relative efficacy of different reinforcers. The effectiveness of CM principles when applied in community-based treatment settings and specifically with clients who have COD remains to be demonstrated.
Some examples of the use of CM techniques have direct implications for people with COD:
- Housing and employment contingent on abstinence. CM, where housing and employment are contingent on abstinence, has been used and studied among populations of homeless persons, many with COD (Milby et al. 1996; Schumacher et al. 1995). Results show that participants in treatment with contingencies were more likely than those in conventional treatment to test clean for drugs, to move into stable housing, and to gain regular employment following treatment.
- Managing benefits and establishing representative payeeships. Procedures have been established to manage benefits for persons with serious mental illness and substance use disorders (Ries and Comtois 1997) and for establishing representative payeeships for clients with COD that involve managing money and other benefits (e.g., Conrad et al. 1999). In these approaches, once abstinence is achieved, clients are allowed greater latitude for management of their own finances.
- A token economy for homeless clients with COD. A token economy has been developed with clients with COD in a shelter to provide
immediate and systematic reinforcement for an array of behaviors during the engagement phase. Points were awarded for the successful accomplishment of a standard list of behaviors essential to the development of commitment, such as medication adherence, abstinence, attendance at program activities, and followthrough on referrals. Points were tallied weekly and tangible rewards (phone cards, treats, toiletries, etc.) were distributed commensurate with the earned point totals (Sacks et al. 2002).
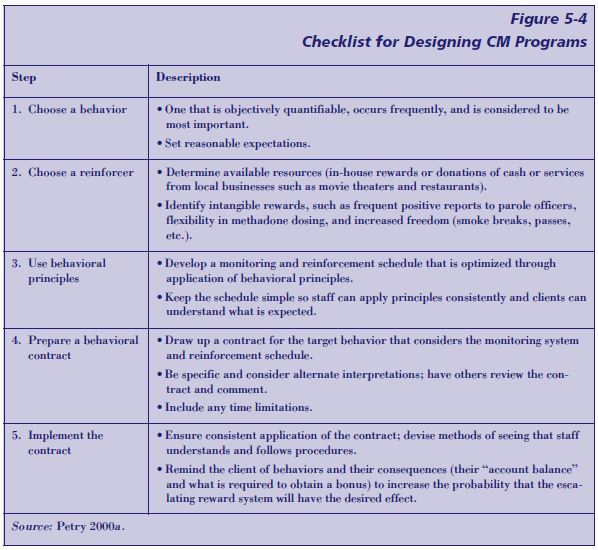
Awareness of the principles of CM can help the clinician to focus on quantifiable behaviors that occur with a good deal of frequency and to provide the reinforcers in an immediate and consistent fashion. CM principles and methods can be accommodated flexibly and applied to a range of new situations that can increase clinician effectiveness. It should be noted that many counselors and programs employ CM principles informally when they praise or reward particular behaviors and accomplishments and that even formal use of CM principles are found in programs where attainment of certain levels and privileges are contingent on meeting certain behavioral criteria.
Case Study: Using CM With a Client With COD
Initial Assessment
Mary A. is a 45-year-old Caucasian woman diagnosed with heroin and cocaine dependence, depression, antisocial personality disorder, and cocaine-induced psychotic episodes. She has a long history of prostitution and sharing injection equipment. She contracted HIV 5 years ago.
Mary A. had been on a regimen of methadone maintenance for about 2 years. Despite dose increases up to 120 mg/day, she continued using heroin at the rate of 1 to 15 bags per day as well as up to 3 to 4 dime bags per day of cocaine. After cessation of a cocaine run, Mary A. experienced tactile and visual hallucinations characterized by “bugs crawling around in my skin.” She mutilated herself during severe episodes and brought in some of the removed skin to show the “bugs” to her therapist.
Mary A. had been hospitalized four times for cocaine-induced psychotic episodes. Following an 11-day stay in an inpatient dual diagnosis program subsequent to another cocaine-induced psychotic episode, Mary A. was referred to an ongoing study of contingency management interventions for methadone-maintained, cocaine-dependent outpatients.
Behaviors To Target
Mary A.’s primary problem was her drug use, which was associated with cocaine-induced psychosis and an inability to adhere to a regimen of psychiatric medications and methadone. Because her opioid and cocaine use were linked intricately, it was thought that a CM intervention that targeted abstinence from both drugs would improve her functioning. As she was already maintained on a high methadone dose, methadone dose adjustments were not made.
CM Plan
Following discharge from the psychiatric unit, Mary A. was offered participation in a NIDA-funded study evaluating lower-cost contingency management treatment (e.g., Petry et al. 2000, pp. 250–257) for cocaine-abusing methadone clients. As part of participation in this study, Mary A. agreed to submit staff-observed urine samples on 2 to 3 randomly selected days each week for 12 weeks. She was told that she had a 50 percent chance of receiving standard methadone treatment plus frequent urine sample testing of standard treatment along with a contingency management intervention. She provided written informed consent, as approved by the University’s Institutional Review Board.
Mary A. was assigned randomly to the CM condition. In this condition, she earned one draw from a bowl for every urine specimen that she submitted that was clean from cocaine or opioids and four draws for every specimen that was clean from both substances. The bowl contained 250 slips of paper. Half of them said “Good job” but did not result in a prize. Other slips stated “small prize” (N=109), “large prize” (N=15), or “jumbo prize” (N=1). Slips were replaced after each drawing so that probabilities remained constant. A lockable prize cabinet was kept onsite in which a variety of small prizes (e.g., socks, lipstick, nail polish, bus tokens, $1 gift certificates to local fast-food restaurants, and food items), large prizes (sweatshirts, portable CD players, watches, and gift certificates to book and record stores), and jumbo prizes (VCRs, televisions, and boom boxes) were kept. When a prize slip was drawn, Mary A. could choose from items available in that category. All prizes were purchased through funds from the research grant.
In addition to the draws from the bowl for clean urine specimens, for each week of consecutive abstinence from both cocaine and opioids Mary A. earned bonus draws. The first week of consecutive cocaine and opioid abstinence resulted in five bonus draws, the second week resulted in six bonus draws, the third week seven and so on. In total, Mary A. could earn about 200 draws if she maintained abstinence throughout the 12-week study.
Clinical Course
Mary A. earned 175 draws during treatment, receiving prizes purchased for a total of $309. She never missed a day of methadone treatment, attended group sessions regularly, and honored all her individual counseling sessions at the clinic. At 6-month follow-up, she had experienced only one drug use lapse, which she self-reported. Her depression cleared with her abstinence, and so did her antisocial behavior. She was pleased with the prizes and stated, “Having good stuff in my apartment and new clothes makes me feel better about myself. When I feel good about me, I don’t want to use cocaine.”
Source: Adapted from Petry et al. 2001b.
Use Cognitive–Behavioral Therapeutic Techniques
Description
Cognitive–behavioral therapy (CBT) is a therapeutic approach that seeks to modify negative or self-defeating thoughts and behavior. CBT is aimed at both thought and behavior change (i.e., coping by thinking differently and coping by acting differently). One cognitive technique is known as “cognitive restructuring.” For example, a client may think initially, “The only time I feel comfortable is when I’m high,” and learn through the counseling process to think instead, “It’s hard to learn to be comfortable socially without doing drugs, but people do so all the time” (TIP 34,
Brief Interventions and Brief Therapies for Substance Abuse [CSAT 1999a], pp. 64–65). CBT includes a focus on overt, observable behaviors—such as the act of taking a drug— and identifies steps to avoid situations that lead to drug taking. CBT also explores the interaction among beliefs, values, perceptions, expectations, and the client’s explanations for why events occurred.
An underlying assumption of CBT is that the client systematically and negatively distorts her view of the self, the environment, and the future (O’Connell 1998). Therefore, a major tenet of CBT is that the person’s thinking is the source of difficulty and that this distorted thinking creates behavioral problems. CBT approaches use cognitive and/or behavioral strategies to identify and replace irrational beliefs with rational beliefs. At the same time, the approach prescribes new behaviors the client practices. These approaches are educational in nature, active and problem-focused, and time-limited.
Advice to the Counselor: Using Contingency Management Techniques
The consensus panel recommends that substance abuse treatment clinicians and programs employ CM techniques with clients with COD in such activities as
- Providing refreshments for attendance at groups or social activities
- Monitoring urine specimens
- Checking medication adherence
- Rewarding clients for obtaining particular goals in their treatment plan
- Reinforcing appropriate verbal and social behavior
CBT for substance abuse
CBT for substance abuse combines elements of behavioral theory, cognitive social learning theory, cognitive theory, and therapy into a distinctive therapeutic approach that helps clients recognize situations where they are likely to use substances, find ways of avoiding those situations, and learn better ways to cope with feelings and situations that might have, in the past, led to substance use (Carroll 1998).
CBT for people with substance use disorders also addresses “coping behaviors.” Coping “refers to what an individual does or thinks in a relapse crisis situation so as to handle the risk for renewed substance use” (Moser and Annis 1996, p. 1101). The approach assumes that “substance abusers are deficient in their ability to cope with interpersonal, social, emotional, and personal problems. In the absence of these skills, such problems are viewed as threatening, stressful, and potentially unsolvable. Based on the individual’s observation of both family members’ and peers’ responses to similar situations and on their own initial experimental use of alcohol or drugs, the individual uses substances as a means of trying to address these problems and the emotional reactions they create” (CSAT 1999a, p. 71). The clinician seeks to help the client increase his coping skills so he will not use drugs in high-stress situations. (See TIP 34 [CSAT 1999a] for a more detailed explanation of the theoretical background of CBT and how it is applied in substance abuse treatment.)
CBT and COD
Distortions in thinking generally are more severe with people with COD than with other substance abuse treatment clients. For example, a person with depression and an alcohol use disorder who has had a bad reaction to a particular antidepressant may claim that all antidepressant medication is bad and must be avoided at all costs. Likewise, individuals may use magnification and minimization to exaggerate the qualities of others, consistently presenting themselves as “losers” who are incapable of accomplishing anything. Clients with COD are, by definition, in need of better coping skills. The Substance Abuse Management Model in the section on Relapse Prevention Therapy later in this chapter provides a pertinent example of how to increase behavioral coping skills.
Grounding
Some clients with COD, such as those who have experienced trauma or sexual abuse, can benefit from a particular coping skill known as “grounding” (Najavits 2002). Many such clients frequently experience overwhelming feelings linked to past trauma, which can be triggered by a seemingly small comment or event. Sometimes, this sets off a craving to use substances. Grounding refers to the use of strategies that soothe and distract the client who is experiencing tidal waves of pain or other strong emotions, helping the individual anchor in the present and in reality. These techniques work by directing the mental focus outward to the external world, rather than inward toward the self. Grounding also can be referred to as “centering,” “looking outward,” “distraction,” or “healthy detachment” (Najavits 2002).
Grounding “can be done anytime, anywhere, by oneself, without anyone else noticing it. It can also be used by a supportive friend or partner who can guide the patient in it when the need arises” (Najavits 2002, p. 125). It is used commonly for PTSD, but can be applied to substance abuse cravings, or any other intense negative feeling, such as anxiety, panic attacks, and rage. Grounding is so basic and simple that it gives even the most impaired clients a useful strategy. However, it must be practiced frequently to be maximally helpful. For a lesson plan and other materials on grounding, see Najavits 2002. See also the section on PTSD in chapter 8 and appendix D of this TIP.
Roles of the client and clinician
CBT is an active approach that works most effectively with persons who are stabilized in the acute phase of their substance use and mental disorders. To be effective, the clinician and the client must develop rapport and a working alliance. The client’s problem is assessed extensively and thorough historical data are collected. Then, collaboratively, dysfunctional automatic thoughts, schemas, and cognitive distortions are identified. Treatment consists of the practice of adaptive skills within the therapeutic environment and in homework sessions. Booster sessions are used following termination of treatment to assist people who have returned to old maladaptive patterns of thinking.
The client with COD is an active participant in treatment, while the role of the clinician is primarily that of educator. The clinician collaborates with the client or group in identifying goals and setting an agenda for each session. The counselor also guides the client by explaining how thinking affects mood and behavior. Clients with COD may need very specific coping skills to overcome the combined challenges of their substance abuse and their mental disorder. For example, Ziedonis and Wyatt (1998, p. 1020) address the need to target “the schizophrenic’s cognitive difficulties (attention span, reading skills, and ability to abstract).” Their approach for these clients includes role-playing to help build communication and problemsolving skills.
Some specific CBT strategies for programs working with clients with COD are described below. See also the text box above for a case example.
Case Study: Using CBT With a Client With COD
Jack W. is referred to the substance abuse treatment agency for evaluation after a positive urine test that revealed the presence of cocaine. He is a 38-year-old African American. Initially, Jack W. engages in treatment in intensive outpatient therapy three times weekly, has clean urine tests, and seems to be doing well. However, after 2 months he starts to appear more depressed, has less to say in group therapy sessions, and appears withdrawn. In a private session with the substance abuse treatment counselor, he says that, “All this effort just isn’t worth it. I feel worse than I did when I started. I might as well quit treatment and forget the job. What’s the point?” The counselor explores what has changed, and Jack W. reveals that his wife has been having a hard time interacting with him as a sober person. Now that he is around the house more than he used to be (he was away frequently, dealing drugs to support his habit), they have more arguments. He feels defeated.
In the vocabulary of CBT, Jack W. demonstrates “all or nothing” thinking (I might as well lose everything because I’m having arguments), overgeneralization, and discounting the positive (he is ignoring the fact that he still has his job, has been clean for 2 months, looks healthier and, until recently, had an improved outlook). His emotionally clouded reasoning is blackening the whole recovery effort, as he personalizes the blame for what he sees as failure to improve his life.
Clearly, Jack W. has lost perspective and seems lost in an apparently overwhelming marital problem. The counselor, using a pad and pencil, draws a circle representing the client and divides it into parts, showing Jack that they represent physical health, his work life, his recovery, risk for legal problems, and family or marriage. He invites Jack to review each one, comparing where he is now and where he was when he first arrived at the clinic in order to evaluate the whole picture. Jack observes that everything is actually getting better with the exception of his marriage. The counselor helps Jack gain the skills needed to stand back from his situation and put a problem in perspective. He also negotiates to determine the kind of help that Jack would see as useful in his marriage. This might be counseling for the couple or an opportunity to practice and rehearse ways of engaging his wife without either of them becoming enraged.
If Jack’s depression continues despite these interventions, the counselor may refer him to a mental health provider for evaluation and treatment of depression.
Use Relapse Prevention Techniques
Description
Marlatt defines relapse as “a breakdown or setback in a person’s attempt to change or modify any target behavior” (1985, p. 3). NIDA elaborates this definition by describing relapse as “any occasion of drug use by recovering addicts that violates their own prior commitment and that often they regret almost immediately” (NIDA 1993, p. 139), and adds Relapse Prevention Therapy (RPT) to its list of effective substance abuse treatment approaches. Relapse can be understood not only as the event of resuming substance use, but also as a process in which indicators of increasing relapse risk can be observed prior to an episode of substance use, or lapse (Daley 1987; Daley and Marlatt 1992).
A variety of relapse prevention models are described in the literature (e.g., Gorski 2000; Marlatt et al. 1999; Monti et al. 1993; NIDA 1993; Rawson et al. 1993). However, a central element of all clinical approaches to relapse prevention is anticipating problems that are likely to arise in maintaining change and labeling them as high-risk situations for resumed substance use, then helping clients to develop effective strategies to cope with those high-risk situations without having a lapse. A key factor in preventing relapse is to understand that relapses are preceded by triggers or cues that signal that trouble is brewing and that these triggers precede exposure to events or internal processes (high-risk situations) where or when resumed substance use is likely to occur. A lapse will occur in response to these high-risk situations unless effective coping strategies are available to the person and are implemented quickly and performed adequately. Clinicians using relapse prevention techniques recognize that lapses (single episodes or brief returns to drug use) are an expected part of overcoming a drug problem, rather than a signal of failure and an indication that all treatment progress has been lost. Therapy sessions aimed at relapse prevention can occur individually or in small groups, and may include practice or role-play on how to cope effectively with high-risk situations.
According to Daley and Marlatt (1992), approaches to relapse prevention have many common elements. Generally they focus on the need for clients to
- Have a broad repertoire of cognitive and behavioral coping strategies to handle high-risk situations and relapse warning signs.
- Make lifestyle changes that decrease the need for alcohol, drugs, or tobacco.
- Increase healthy activities.
- Prepare for interrupting lapses, so that they do not end in full-blown relapse.
- Resume or continue to practice relapse prevention skills even when a full-blown relapse does occur by renewing their commitment to abstinence rather than giving up the goal of living a drug-free life.
RPT is an intervention designed to teach individuals who are trying to maintain health behavior changes how to anticipate and cope with the problem of relapse (Marlatt 1985). RPT strategies can be placed in five categories: Assessment Procedures, Insight/ Awareness Raising Techniques, Coping Skills Training, Cognitive Strategies, and Lifestyle Modification (Marlatt 1985). RPT Assessment Procedures are designed to help clients appreciate the nature of their problems in objective terms, to measure motivation for change, and to identify risk factors that increase the probability of relapse. Insight/Awareness Raising Techniques are designed to provide clients with alternative beliefs concerning the nature of the behavior change process (e.g., to view it as a learning process) and, through self-monitoring, to help clients identify patterns of emotion, thought, and behavior related to both substance use and co-occurring mental disorders. Coping Skills Training strategies include teaching clients behavioral and cognitive strategies. Cognitive Strategies are used to manage urges and craving, to identify early warning signals, and to reframe reactions to an initial lapse. Finally, Lifestyle Modification Strategies (e.g., meditation and exercise) are designed to strengthen clients’ overall coping capacity.
Adapting CBT for Clients With COD
- Use visual aids, including illustrations and concept mapping (a visual presentation of concepts that makes patterns evident).
- Practice role preparation and rehearse for unexpected circumstances.
- Provide specific in vivo feedback on applying principles and techniques.
- Use outlines for all sessions that list specific behaviorally anchored learning objectives.
- Test for knowledge acquisition.
- Make use of memory enhancement aids, including notes, tapes, and mnemonic devices.
Source: Adapted from Peters and Hills 1997.
In Marlatt’s model of RPT, lapses are seen as a “fork in the road” or a “crisis.” Each lapse contains the dual elements of “danger” (progression to full-blown relapse) and “opportunity” (reduced relapse risk in the future due to the lessons learned from debriefing the lapse). The goal of effective RPT is to teach clients to recognize increasing relapse risk and to intervene at earlier points in the relapse process in order to encourage clients to progress toward maintaining abstinence from drugs and living a life in which lapses occur less often and are less severe.
Specific aspects of RPT might include
- Exploring with the client both the positive and negative consequences of continued drug use (“decisional balance,” as discussed in the motivational interviewing section of this chapter)
- Helping clients to recognize high-risk situations for returning to drug use
- Helping clients to develop the skills to avoid those situations or cope effectively with them when they do occur
- Developing a “relapse emergency plan” in order to exercise “damage control” to limit the duration and severity of lapses
- Learning specific skills to identify and cope effectively with drug urges and craving
Clients also are encouraged to begin the process of creating a more balanced lifestyle to manage their COD more effectively and to fulfill their needs without using drugs to cope with life’s demands and opportunities. In the treatment of clients with COD, it often is critical to consider adherence to a medical regimen required to manage disruptive and disorganizing symptoms of mental disorder as a relapse issue. In terms of medication adherence, a “lapse” is defined as not taking the prescribed drugs one needs rather than the resumption of taking illicit drugs for self-medication or pleasure seeking.
Empirical evidence related to relapse prevention therapy
Carroll (1996) reviewed 24 randomized controlled trials of RPT among smokers and abusers of alcohol, marijuana, cocaine, opioids, and other drugs. While many of the studies were of smokers—in which Carroll noted the strongest support for RPT in terms of improved outcomes for relapse severity, durability of effects, and client-treatment matching, as compared to no-treatment controls—comparable results were found for alcohol and illicit drugs as well. Of particular importance was the observation that the positive effects of RPT treatment were greater among those with higher severities of both psychiatric symptoms and addiction impairment, which suggests the technique would be helpful in the treatment of clients with COD.
In a meta-analytic review of 26 published and unpublished studies using Marlatt’s RPT model, Irvin et al. (1999) found that RPT generally was effective particularly for alcohol problems and was most effective when applied to alcohol or polysubstance use disorders, combined with medication. The efficacy of RPT has been demonstrated sufficiently to be included by NIDA (1999a) as a recommended approach “to supplement or enhance—not replace—existing treatment programs” (p. 35).
Advice to the Counselor: Using Relapse Prevention Methods
The consensus panel recommends using the following relapse prevention methods with clients with COD:
- Provide relapse prevention education on both mental disorders and substance abuse and their interrelations.
- Teach skills to help the client handle pressure for discontinuing psychotropic medication and to increase medication adherence.
- Encourage attendance at dual recovery groups and teach social skills necessary for participation.
- Use daily inventory to monitor psychiatric symptoms and symptoms changes.
- If relapse occurs, use it as a learning experience to investigate triggers with the client. Reframe the relapse as an opportunity for self-knowledge and a step toward ultimate success.
Adaptations for clients with COD
Several groups have developed relapse prevention interventions aimed at clients with different mental disorders or substance use diagnoses (see Evans and Sullivan 2001). Weiss and colleagues (1998) developed a 20-session relapse prevention group therapy for the treatment of clients with co-occurring bipolar and substance use disorders. This group stressed concepts of importance to both disorders—for example, it contrasts “may as well” thinking, which allows for relapse and failure to take medication, with “it matters what you do.” It also teaches useful skills relevant to both disorders, such as coping with high-risk situations and modifying lifestyle to improve self-care (p. 49). Ziedonis and Stern (2001) have developed a dual recovery therapy, which blends traditional
mental health and addiction treatments (including both motivational enhancement therapy and relapse prevention) for clients with serious mental illness. Also, Nigam and colleagues (1992) developed a relapse prevention group for clients with COD.
Substance abuse management module
Roberts et al. (1999) developed The Substance Abuse Management Module (SAMM) based on the previously described RPT approach of Marlatt and his colleagues. SAMM originally was designed to be a component of a comprehensive approach to the treatment of co-occurring substance use dependence and schizophrenia. This detailed treatment manual illustrates many RPT
techniques and focuses on the most common problems encountered by clients with severe COD. SAMM offers a detailed cognitive– behavioral strategy for each of several common problems that clients face. Each strategy includes both didactics and detailed skills training procedures including role-play practice. Emphasis is placed on rehearsing such key coping behaviors as refusing drugs, negotiating with treatment staff, acting appropriately at meetings for mutual self-help, and developing healthy habits. Both counselor and client manuals are available.
The text box beginning on p. 131 describes the SAMM protocol (Roberts et al. 1999) shows how a clinician might work with a substance abuse treatment client with COD to help the client avoid drugs.
Integrated treatment
RPT (Marlatt and Gordon 1985) and other cognitive–behavioral approaches to psychotherapy and substance abuse treatment allow clinicians to treat COD in a integrated way by
- Doing a detailed functional analysis of the relationships between substance use, Axis I or II symptoms, and any reported criminal conduct
- Evaluating the unique and common high-risk factors for each problem and determining their interrelationships
- Assessing both cognitive and behavioral coping skills deficits
- Implementing both cognitive and behavioral coping skills training tailored to meet the specific needs of an individual client with respect to all three target behaviors (i.e., substance use, symptoms of mental disorder, and criminal conduct)
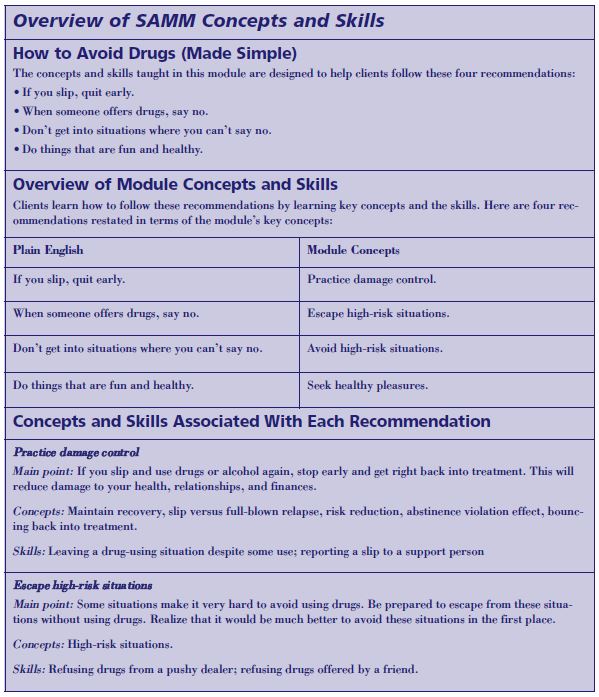
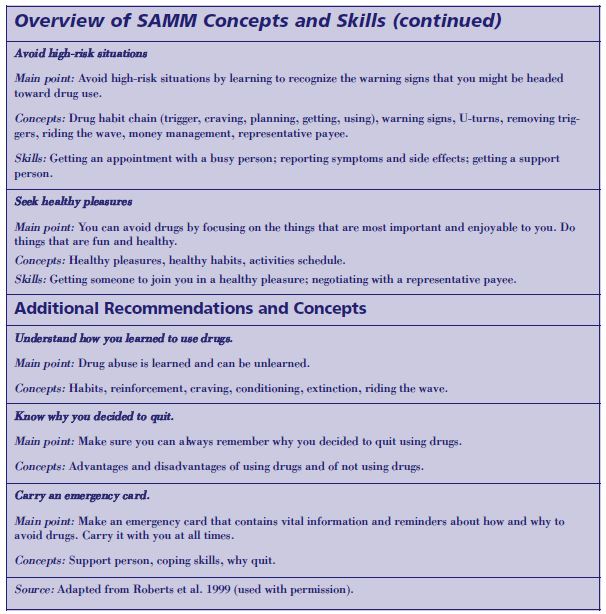
Summary of RP strategies for clients with COD
Daley and Lis (1995) summarize RP strategies that can be adapted for clients with COD, some of which are listed below:
- Regardless of the client’s motivational level or recovery stage, relapse education should be provided and related to the individual’s mental disorder. The latter is important, particularly because the pattern typically followed by clients with COD begins with an increase in substance use leading to lowered efficacy or discontinuation of psychiatric medication, or missed counseling sessions. As a consequence, symptoms of mental disorders reappear or worsen, the client’s tendency to self-medicate through substance use is exacerbated, and the downward spiral is perpetuated.
- Clients with COD need effective strategies to cope with pressures to discontinue their prescribed psychiatric medication. One such strategy simply is to prepare clients for external pressure from other people to stop taking their medications. Rehearsing circumstances in which this type of pressure is applied, along with anticipating the possibility, enables clients with COD to react appropriately. Reinforcing the difference between substances of abuse—getting “high”—and taking psychiatric medication to treat an illness is another simple but effective strategy.
- An integral component of recovery is the use of mutual self-help and dual recovery groups to provide the support and understanding of shared experience. To maximize the effectiveness of their participation, clients with COD usually need help with social skills (listening, self-disclosure, expressing feelings/desires, and addressing conflict).
Clients can use daily self-ratings of persistent psychiatric symptoms to monitor their status. Use of the daily inventory and symptom review should be encouraged to help clients with COD to track changes and take action before deteriorating status becomes critical. See the text box on p. 134 for a case study applying RP strategies.
Use Repetition and Skills-Building To Address Deficits in Functioning
In applying the approaches described above, keep in mind that clients with COD often have cognitive limitations, including difficulty concentrating. Sometimes these limitations are transient and improve during the first several weeks of treatment; at other times, symptoms persist for long periods. In some cases, individuals with specific disorders (schizophrenia, attention deficit disorder) may manifest these symptoms as part of their disorder.
General treatment strategies to address cognitive limitations in clients include being more concrete and less abstract in communicating ideas, using simpler concepts, having briefer discussions, and repeating the core concepts many times. In addition, individuals often learn and remember better if information is presented in multiple formats (verbally; visually; or affectively through stories, music, and experiential activities). Role-playing real-life situations also is a useful technique when working with clients with cognitive limitations. For example, a client might be assigned to practice “asking for help” phone calls using a prepared script. This can be done individually with the counselor coaching, or in a group, to obtain feedback from the members.
When compared to individuals without additional disorders or disabilities, persons with COD and additional deficits often will require more substance abuse treatment in order to attain and maintain abstinence. A primary reason for this is that abstinence requires the development and utilization of a set of recovery skills, and persons with mental disorders often have a harder time learning new skills. They may require more support in smaller steps with more practice, rehearsal, and repetition. The challenge is not to provide more intensive or more complicated treatment for clients with COD, but rather to tailor the process of acquiring new skills to the needs and abilities of the client.
Case Study: Preventing Relapse in a Client With COD
Stan Z. is a 32-year-old with diagnoses of recurrent major depression, antisocial personality disorder, crack/cocaine dependence, and polysubstance abuse. He has a 15-year history of addiction, including a 2-year history of crack addiction. Stan Z. has been in a variety of psychiatric and substance abuse treatment programs during the past 10 years. His longest clean time has been 14 months. He has been attending a dual-diagnosis outpatient clinic for the past 9 months and going to Narcotics Anonymous (NA) meetings off and on for several years. Stan Z. has been clean from all substances for 7 months. Following is a list of high-risk relapse factors and coping strategies identified by Stan Z. and his counselor:
High-Risk Factor 1
Stan Z. is tired and bored “with just working, staying at home and watching TV, or going to NA meetings.” Recently, he has been thinking about how much he “misses the action of the good old days” of hanging with old friends and does not think he has enough things to do that are interesting.
Possible coping strategies for Stan Z. include the following: (1) remind him of problems caused by hanging out with people who use drugs and using drugs by writing out a specific list of problems associated with addiction; (2) challenge the notion of the “good old days” by looking closely at the “bad” aspects of those days; (3) remind him of how far he has come in his recent recovery, especially being able to get and keep a job, maintain a relationship with one woman, and stay out of trouble with the law; (4) discuss current feelings and struggles with an NA sponsor and NA friends to find out how they handled similar feelings and thoughts; and (5) make a list of activities that will not threaten recovery and can provide a sense of fun and excitement and plan to start active involvement in one of these activities.
High-Risk Factor 2
Stan Z. is getting bored with his relationship with his girlfriend. He feels she is too much of a “home body” and wants more excitement in his relationship with her. He also is having increased thoughts of having sex with other women.
Possible coping strategies for Stan Z. include the following: (1) explore in therapy sessions why he is really feeling bored with his girlfriend, noting he has a long-standing pattern of dumping girlfriends after just a few months; (2) challenge his belief that the problem is mainly his girlfriend so that he sees how his attitudes and beliefs play a role in this problem; (3) talk directly with his girlfriend in a nonblaming fashion about his desire to work together to find ways to instill more excitement in the relationship; (4) remind him of potential dangers of casual sex with a woman he does not know very well and that he cannot reach his goal of maintaining a meaningful, mutual relationship if he gets involved sexually with another woman. His past history is concrete proof that such involvement always leads to sabotaging his primary relationship.
High-Risk Factor 3
Stan Z. wants to stop taking antidepressant medications. His mood has been good for several months and he does not see the need to continue medications.
Possible coping strategies include the following: (1) discuss his concern about medications with his counselor and psychiatrist before making a final decision; (2) review with his treatment team the reasons for being on antidepressant medications; (3) remind him that because he had several episodes of depression, even during times when he has been drug-free for a long period, medication can help “prevent” the likelihood of a future episode of depression.
Source: Daley and Lis 1995, pp. 255–256.
Case Study: Using Repetition and Skills Building With a Client With COD
In individual counseling sessions with Susan H., a 34-year-old Caucasian woman with bipolar disorder and alcohol dependence, the counselor observes that often she is forgetful about details of her recent past, including what has been said and agreed to in therapy. Conclusions the counselor thought were clear in one session seem to be fuzzy by the next. The counselor begins to start sessions with a brief review of the last session. He also allows time at the end of each session to review what has just happened. As Susan H. is having difficulty remembering appointment times and other responsibilities, he helps her devise a system of reminders in big letters on her refrigerator.
Facilitate Client Participation in Mutual Self-Help Groups
Just as the strategies discussed in this chapter have proven helpful both to clients who have only substance use disorders as well as to those with COD, so the use of mutual self-help groups is a key tool for the clinician in assisting both categories of clients. In addition to traditional 12-Step groups, dual recovery mutual self-help approaches are becoming increasingly common in most large communities. The clinician plays an important role in helping clients with COD access appropriate mutual self-help resources and benefit from them. (See chapter 7 for an extended presentation of Dual Recovery Mutual Self-Help approaches tailored to meet the needs of persons with COD.) Groups for those who do not speak English may not be available, and the clinician is advised to seek resources in other counties or, if the number of clients warrants it, to initiate organization of a group for those who speak the same non-English language.
The clinician can assist the client by:
- Helping the client locate an appropriate group. The clinician should strive to be aware not only of what local 12-Step and other dual recovery mutual self-help groups meet in the community, but also which 12-Step groups are known to be friendly to clients with COD, have other members with COD, or are designed specifically for people with COD. Clinicians do this by visiting groups to see how they are conducted, collaborating with colleagues to discuss groups in the area, updating their own lists of groups periodically, and gathering information from clients. The clinician should ensure that the group the client attends is a good fit for the client in terms of the age, gender, and cultural factors of the other members. In some communities, alternatives to 12-Step groups are available, such as Secular Organizations for Sobriety.
- Helping the client find a sponsor, ideally one who also has COD and is at a later stage of recovery. Knowing that he or she has a sponsor who truly understands the impact of two or more disorders will be encouraging for the client. Also, some clients may “put people off” in a group and have particular difficulty finding a sponsor without the clinician’s support.
- Helping the client prepare to participate appropriately in the group. Some clients, particularly those with serious mental illness or anxiety about group participation, may need to have the group process explained ahead of time. Clients should be told the structure of a meeting, expectations of sharing, and how to participate in the closing exercises, which may include holding hands and repeating sayings or prayers. They may need to rehearse the kinds of things that are and are not appropriate to share at such meetings. Clients also should be taught how to “pass” and when this would be appropriate. The counselor should be familiar enough with group function and dynamics to actually “walk the client” through the meeting before attending.
- Helping overcome barriers to group participation. The clinician should be aware of the genuine difficulties a client may have in connecting with a group. While clients with COD, like any others, may have some resistance to change, they also may have legitimate barriers they cannot remove alone. For example, a client with cognitive difficulties may need help working out how he or she can physically get to the meeting. The counselor may need to write down very detailed instructions for this person that another client would not need (e.g., “Catch the number 9 bus on the other side of the street from the treatment center, get off at Main Street, and walk three blocks to the left to the white church. Walk in at the basement entrance and go to Room 5.”)
- Debriefing with the client after he or she has attended a meeting to help process his or her reactions and prepare for future attendance. The clinician’s work does not end with referral to a mutual self-help group. The clinician must be prepared to help the client overcome any obstacles after attending the first group to ensure engagement in the group. Often this involves a discussion of the client’s reaction to the group and a clarification of how he or she can participate in future groups.
Case Study: Helping a Client Find a Sponsor
Linda C. had attended her 12-Step group for about 3 months, and although she knew she should ask someone to sponsor her, she was shy and afraid of rejection. She had identified a few women who might be good sponsors, but each week in therapy she stated that she was afraid to reach out, and no one had approached her, although the group members seemed “friendly enough.” The therapist suggested that Linda C. “share” at a meeting, simply stating that she’d like a sponsor but was feeling shy and didn’t want to be rejected. The therapist and Linda C. role-played together in a session, and the therapist reminded Linda C. that it was okay to feel afraid and if she couldn’t share at the next meeting, they would talk about what stopped her.
After the next meeting, Linda C. related that she almost “shared” but got scared at the last minute, and was feeling bad that she had missed an opportunity. They talked about getting it over with, and Linda C. resolved to reach out, starting her sharing statement with, “It’s hard for me to talk in public, but I want to work this program, so I’m going to tell you all that I know it’s time to get a sponsor.” This therapy work helped Linda C. to put her need out to the group, and the response from group members was helpful to Linda C., with several women offering to meet with her to talk about sponsorship. This experience also helped Linda C. to become more attached to the group and to learn a new skill for seeking help. While Linda C. was helped by counseling strategies alone, others with “social phobia” also may need antidepressant
medications in addition to counseling.

