In This Chapter…
- The Evolving Field of Co-Occurring Disorders
- Important Developments That Led to This TIP
- Organization of This TIP
Overview
Over the past few decades, practitioners and researchers increasingly have recognized the link between substance abuse and mental disorders. Treatment Improvement Protocol (TIP) 9,Assessment and Treatment of Patients With Coexisting Mental Illness and Alcohol and Other Drug Abuse (Center for Substance Abuse Treatment [CSAT] 1994a ), answered the treatment field’s need for an overview of diagnostic criteria, assessment, psychopharmacology, specific mental disorders, and the need for linkage between the mental health services system and substance abuse treatment system.
Subsequent to TIP 9, research has provided a more in-depth understanding of co-occurring substance use and mental disorders—how common they are, the multiple problems they create, and the impact they have on treatment and treatment outcome. As knowledge of co-occurring disorders (COD) continues to evolve, new challenges arise: How do we treat specific populations such as the homeless and those in our criminal justice system? What is the role of housing? What about those with specific mental disorders such as posttraumatic stress disorder? Where is the best locus for treatment? Can we build an integrated system of care? The main purpose of this TIP is to provide addiction counselors and other practitioners with this state-of-the-art information on the rapidly advancing field of co-occurring substance use and mental disorders.
Following a discussion of the evolving field of co-occurring disorders, this chapter addresses the developments that led to this TIP. It then describes the scope of this TIP (both what is included and what is excluded by design), its intended audience, and the basic approach that has guided the selection of strategies, techniques, and models highlighted in the text. The organization of the TIP is laid out for the reader, with the components of each chapter and appendix described in an effort to help users of the TIP quickly locate subjects of immediate interest.
The Evolving Field of Co-Occurring Disorders
Today’s emphasis on the relationship between substance use and mental disorders dates to the late 1970s, when practitioners increasingly became aware of the implications of these disorders, when occurring together, for treatment outcomes. The association between depression and substance abuse was particularly striking and became the subject of several early studies (e.g., Woody and Blaine 1979). In the 1980s and 1990s, however, both the substance abuse and mental health communities found that a wide range of mental disorders were associated with substance abuse, not just depression (e.g.,De Leon 1989; Pepper et al. 1981; Rounsaville et al. 1982b ; Sciacca 1991). During this period, substance abuse treatment programs typically reported that 50 to 75 percent of clients had co-occurring mental disorders, while clinicians in mental health settings reported that between 20 and 50 percent of their clients had co-occurring substance use disorders. (See Sacks et al. 1997b for a summary of studies.)
The multiple studies reflect the extent to which COD constitutes a clinical concern. At the same time, however, these studies varied in that they (1) were conducted in an array of settings and on a range of sample sizes from 68 to 20,291, (2) used different measures and criteria for determining a disorder, and (3) reported on different time periods (i.e., either lifetime or current, or both). This diversity in reporting can produce differing estimates and suggests a need to address the broad range of survey and analytic strategies used to generate estimates. Further work to clarify the type, severity, and clinical significance of cooccurring disorders can contribute to an improved understanding of the phenomenon and treatment. Nevertheless, it is important that, in spite of those differences, there is a consistency in reporting significant rates of disorder across all studies.
Researchers not only found a link between substance abuse and mental illness, they also found the dramatic impact the complicating presence of substance abuse may have on the course of treatment for mental illness. One study of 121 clients with psychoses found that those with substance abuse problems (36 percent) spent twice as many days in the hospital over the 2 years prior to treatment as clients without substance abuse problems (Crome 1999; Menezes et al. 1996). These clients often have poorer outcomes, such as higher rates of HIV infection, relapse, rehospitalization, depression, and suicide risk (Drake et al. 1998b ; Office of the Surgeon General 1999).
Researchers also have clearly demonstrated that substance abuse treatment of clients with co-occurring mental illness and substance use disorders can be beneficial—even for clients with serious mental disorders. For example, the National Treatment Improvement Evaluation Study (NTIES) found marked reductions in suicidality the year following substance abuse treatment compared to the year prior to treatment for adults, young adults, adolescents, and subgroups of abused and nonabused women. Suicide attempts declined about four fifths for both the 3,037 male clients and the 1,374 female clients studied (Karageorge 2001). Many clients in traditional substance abuse treatment settings who had mild to moderate mental disorders were found to do well with traditional substance abuse treatment methods (Hser et al. 2001; Hubbard et al. 1989; Joe et al. 1995; Simpson et al. 2002; Woody et al. 1991). However, modifications designed to address mental disorders may further enhance treatment effectiveness and can be essential for people with severe mental disorders. This TIP will discuss the modifications and approaches practitioners have found to be helpful. For examples, see the sections on suicide assessment and intervention in chapter 8 and appendix D.
Just as the field of treatment for substance use and mental disorders has evolved to become more precise, so too has the terminology used to describe people with both substance use and mental disorders. The term co-occurring disorders replaces the terms dual disorder or dual diagnosis. These latter terms, though used commonly to refer to the combination of substance use and mental disorders, are confusing in that they also refer to other combinations of disorders (such as mental disorders and mental retardation). Furthermore, the terms suggest that there are only two disorders occurring at the same time, when in fact there may be more. For purposes of this TIP, co-occurring disorders refers to co-occurring substance use (abuse or dependence) and mental disorders. Clients said to have co-occurring disorders have one or more disorders relating to the use of alcohol and/or other drugs of abuse as well as one or more mental disorders. A diagnosis of co-occurring disorders occurs when at least one disorder of each type can be established independent of the other and is not simply a cluster of symptoms resulting from the one disorder. (See chapter 2 for more discussion of terminology used in this TIP.)
New models and strategies are receiving attention and encouraging treatment innovation (Anderson 1997; De Leon 1996; Miller 1994a ; Minkoff 1989; National Advisory Council [NAC] 1997; Onken et al. 1997; Osher and Drake 1996). Reflecting the increased interest in issues surrounding effective treatment for this population, the American Society of Addiction Medicine (ASAM) added substantial new sections on clients with COD to an update of its patient placement criteria. These sections refine criteria both for placing clients with COD in treatment and for establishing and operating programs to provide services for such clients (ASAM 2001).
In another important development, the National Association of State Alcohol and Drug Abuse Directors (NASADAD) began surveying its members about effective treatment of clients with COD in their States (Gustafson et al. 1999). In addition, NASADAD has joined with the National Association of State Mental Health Program Directors (NASMHPD) (NASMHPD-NASADAD 1999, 2000) and other collaborators in a series of national efforts designed to
-
Foster improvement in treatment by emphasizing the importance of knowledge of both mental health and substance abuse treatment when working with clients for whom both issues are relevant.
-
Provide a classification of treatment settings to facilitate systematic planning, consultations, collaborations, and integration.
-
Reduce the stigma associated with both disorders and increase the acceptance of substance abuse and mental health concerns as a standard part of healthcare information gathering.
These efforts are slowly changing the way that the public, policymakers, and substance abuse counselors view mental illness. Still, stigma attached to mental illness remains. One topic worth mentioning is the public perception that people with mental illness are dangerous and pose a risk of violence. However, studies have shown that the public’s fear is greater than the actual risk, and that often, people with mental disorders are not particularly violent; it is when substance abuse is added that violence can ensue. For example, Steadman et al. (1998) found that substance abuse symptoms significantly raised the rate of violence in both individuals with mental illness and those without mental illness. This research adds support to the importance of treating both mental illness and substance abuse.
Researchers have clearly demonstrated that substance abuse treatment of clients with cooccurring mental illness and substance use disorders can be beneficial.
In recent years, dissemination of knowledge has been widespread. Numerous books and hundreds of articles have been published, from counseling manuals and instruction (Evans and Sullivan 2001; Pepper and Massaro 1995) to database analysis of linkage among treatment systems and payors (Coffey et al. 2001). Several annual “dual diagnosis” conferences emerged. One of the most longstanding is the annual conference on The Person With Mental Illness and Substance Abuse, hosted by MCP Hahnemann University (now Drexel University), which began in 1988.
In spite of these developments, individuals with substance use and mental disorders commonly appear at facilities that are not prepared to treat them. They may be treated for one disorder without consideration of the other disorder, often “bouncing” from one type of treatment to another as symptoms of one disorder or another become predominant. Sometimes they simply “fall through the cracks” and do not receive needed treatment. This TIP captures the current state-of-the-art treatment strategies to assist counselors and treatment agencies in providing appropriate services to clients with COD.
Important Developments That Led to This TIP
Important developments in a number of areas pointed to the need for a revised TIP on co-occurring disorders. Among the factors that contributed to the need for this document are the availability of significant data on the prevalence of COD, the emergence of new treatment populations with COD (such as people who are homeless, people with HIV/AIDS, and persons in the criminal justice system), and changes in treatment delivery (including an increasing number of programs serving persons with COD). The following section provides a summary of data relevant to each of these key areas.
The Availability of Prevalence and Other Data
Prevalence and other data on COD have established the scope and impact of the problem, and the need for appropriate treatment and services. Four key findings are borne out by prevalence and other available data, each of which is important in understanding the challenges of providing effective treatment to this population.
(1) COD are common in the general adult population, though many individuals with COD go untreated.
National surveys suggest COD are common in the adult population. For example, the National Survey on Drug Use and Health (NSDUH) reports that in 2002, 4 million adults met the criteria for both serious mental illness (SMI) and substance dependence and abuse. NSDUH information is based on a sample of 67,500 American civilians aged 12 or older in noninstitutionalized settings (Office of Applied Studies [OAS] 2003). The NSDUH defined SMI as having at some time during the past year a diagnosable mental, behavioral, or emotional disorder that met the criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) (American Psychiatric Association 1994) and resulted in functional impairment that substantially interfered with or limited one or more major life activities. The NSDUH classification scheme was not diagnosis specific, but function specific. Results from the survey are highlighted below.
-
SMI is highly correlated with substance dependence or abuse. Among adults with SMI in 2002, 23.2 percent were dependent on or abused alcohol or illicit drugs, while the rate among adults without SMI was only 8.2 percent. Among adults with substance dependence or abuse, 20.4 percent had SMI; the rate of SMI was 7 percent among adults who were not dependent on or abusing a substance.
-
Among adults who used an illicit drug in the past year, 17.1 percent had SMI in that year, while the rate was 6.9 percent among adults who did not use an illicit drug. Conversely, among adults with SMI, 28.9 percent used an illicit drug in the past year while the rate was 12.7 percent among those without SMI (OAS 2003b).
-
SMI was correlated with binge alcohol use (defined as drinking five or more drinks on the same occasion on at least one day in the past 30 days). Among adults with SMI, 28.8 percent were binge drinkers, while 23.9 percent of adults with no SMI were binge drinkers.
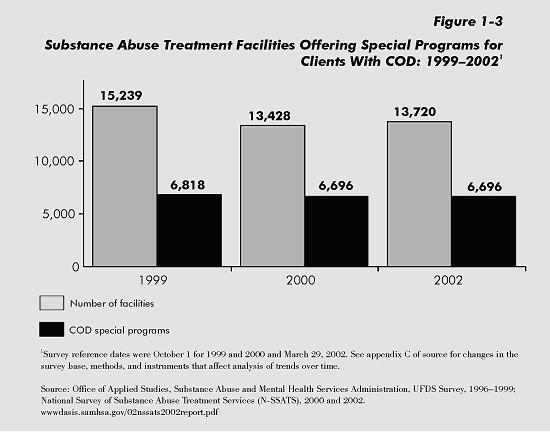
Earlier, the National Comorbidity Study (NCS) reported 1991 information on mental disorders and substance abuse or dependence in a sample of 8,098 American civilians aged 15 to 54 in noninstitutionalized settings. Figure 1-1 shows estimates from the NCS of the comparative number of any alcohol, drug abuse, or mental disorder (52 million), any mental disorder (40 million), any substance abuse/dependence disorder (20 million), and both mental disorder and substance abuse/dependence (8 million) in the past year.
In a series of articles derived from the NCS, Kessler and colleagues give a range of estimates related to both the lifetime and 12-month prevalence of COD (Kessler et al. 1994, 1996a , b , 1997). They estimate that 10 million Americans of all ages and in both institutional and noninstitutional settings have COD in any given year. Kessler et al. also estimate the lifetime prevalence of COD (not shown in Figure 1-1, which relates only the prevalence in the past 12 months) (1996a, p. 25) as follows: “…51 percent of those with a lifetime addictive disorder also had a lifetime mental disorder, compared to 38 percent in the ECA.” (The ECA—Epidemiologic Catchment Area study—predated the NCS study; this National Institute of Mental Health study of 20,291 people was representative of the total U.S. community and institutional populations [Regier et al. 1990]).
Comparative figures for individuals with COD whose addictive disorders involve alcohol versus drugs are also available. Fifty-three percent of the respondents with lifetime alcohol abuse or dependence also had one or more lifetime mental disorders. For respondents with lifetime illicit drug abuse/dependence, 59 percent also had a lifetime mental disorder, and 71 percent of those with lifetime illicit drug abuse/dependence had alcohol abuse or dependence over their lifetime (Office of the Inspector General 1995).
Research suggests that the likelihood of seeking treatment is strongly increased in the presence of at least one co-occurring condition.
A recent first report from the National Comorbidity Survey Replication, conducted between February 2001 and December 2002 (Kessler and Walters 2002), provides more precise information on rates of specific disorders. For example, rates of major depressive disorder were reported at 6.6 percent in the general population in the last year, or an estimated number between 13.1 and 14.2 million people (Kessler et al. 2003b ). Additional data from a new and expanded NCS survey are now available (e.g., Breslau et al. 2004a , b ; Kessler 2003; Kessler et al. 2003a ; see also the Web site www.hcp.med.harvard.edu/ncs).
Research suggests that the likelihood of seeking treatment is strongly increased in the presence of at least one co-occurring condition. The National Longitudinal Alcohol Epidemiologic Study (NLAES)—a nationwide household survey of 42,862 respondents aged 18 or older conducted by the National Institute on Alcohol Abuse and Alcoholism—reveals that a large increase in treatment for an alcohol disorder and a drug disorder occurs when there is a co-occurring “major depressive disorder” (Grant 1997). NCS data suggest that people with more than two disorders are more likely to receive treatment than those with “only” two. People with three or more diagnosable conditions were the most likely to be severely impaired and to require hospitalization (NAC 1997).
While people with co-occurring disorders are more likely to seek treatment, research consistently shows a gap between the number of people who are identified in a survey as having a disorder and the number of people receiving any type of treatment. Even of those with three or more disorders, a troubling 60 percent never received any treatment (Kessler et al. 1994; NAC 1997). Based on NLAES data, Grant (1997, p. 13) notes that one of the most interesting results of the survey is the “sheer number of respondents with alcohol and drug use disorders missing from the treated population. Only 9.9 percent and 8.8 percent of the respondents classified with past-year alcohol and drug use disorders, respectively, sought treatment.”
(2) Some evidence supports an increased prevalence of people with COD and of more programs for people with COD.
NASADAD conducts voluntary surveys of State Alcohol and Drug Abuse Agencies and produces the State Alcohol and Drug Abuse Profile (SADAP) reports. In 1996, NASADAD asked the States to describe any special programs in their States for clients with COD and to provide any available fiscal year (FY) 1995 statistics on the number of “dually diagnosed” clients treated (Gustafson et al. 1997). Forty-one States plus Palau, Puerto Rico, and the U.S. Virgin Islands responded. About 3 years later, 31 States responded to a request for detailed statistics on the number of persons admitted in FYs 1996 and 1997 to programs for treatment of COD (Gustafson et al. 1999). In general, examination of SADAP State profiles for information related to COD suggests about a 10 percent increase since the NASADAD survey in both the number of people with COD entering treatment and in the number of programs in many States over that 3-year period (Gustafson et al. 1999).
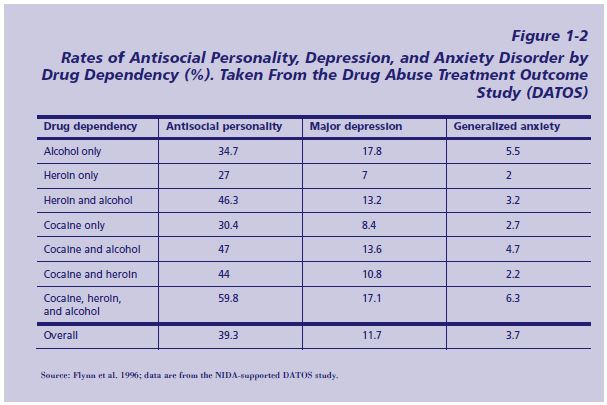
The 2002 National Survey of Substance Abuse Treatment Services (N-SSATS) indicated that about 49 percent of 13,720 facilities nationwide reporting substance abuse services offered programs or groups for those with COD (OAS 2003a ). However, only 38 percent of the 8,292 responding facilities that focused primarily on substance abuse offered such COD programming. Sixty-three percent of the 1,126 responding mental health services that offered substance abuse services offered COD programs or groups. About 70 percent of the 3,440 facilities that have a mix of mental health and substance abuse treatment services offer COD programs or groups.
Still it must be kept in mind that of all the approximately 1.36 million clients in treatment for substance use disorders in 2002, about 68 percent were treated in facilities whose primary focus was substance abuse services and 23 percent were treated in facilities whose focus was a mix of both mental health and substance abuse services. Only 4 percent of these individuals were in facilities whose primary focus was the provision of mental health services.
(3) Rates of mental disorders increase as the number of substance use disorders increasse, further complicating treatment.
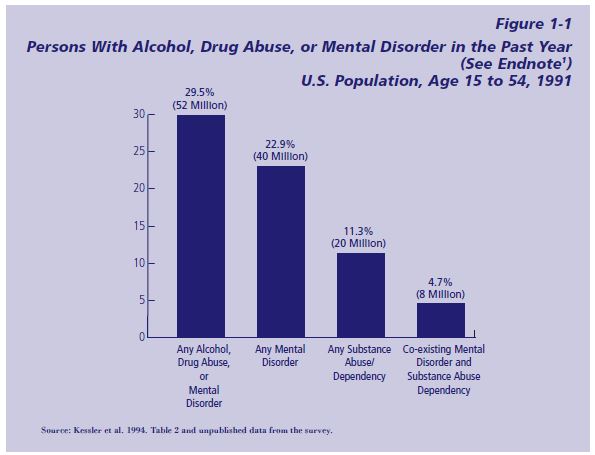
In their analysis of data from a series of studies supported by the National Institute on Drug Abuse, the Drug Abuse Treatment Outcome Study (DATOS), Flynn et al. (1996) demonstrate that the likelihood of mental disorders rises with the increasing number of substance dependencies. Participating clients were assessed according to DSM-III-R criteria (Diagnostic and Statistical Manual for Mental Disorders, 3d edition revised) for lifetime antisocial personality, major depression, generalized anxiety disorder, and/or any combination of these disorders.
DATOS was a national study of clients entering more than 90 substance abuse treatment programs in 11 metropolitan areas, mainly during 1992 (Flynn et al. 1997). Of the initial intake sample of 10,010 clients, 7,402 completed an intake and a clinical assessment interview and met DSM-III-R criteria for dependence on alcohol, cocaine, and/or heroin. Figure 1-2 shows a general trend of increase in the rates of DSM-III-R lifetime antisocial personality disorder, major depression, and generalized anxiety disorder as the number of substance dependencies involving alcohol, heroin, and cocaine increases (except for the relationship between alcohol dependence only and major depression and generalized anxiety). Since the use of multiple drugs is common in those with substance use disorders, treatment is further complicated for these people by the greater incidence of mental disorders that accompanies multiple drug use.
(4) Compared to people with mental or substance use disorders alone, people with COD are more likely to be hospitalized. Some evidence suggests that the rate of hospitalization for people with COD is increasing.
According to Coffey and colleagues, the rate of hospitalization for clients with both a mental and a substance use disorder was more than 20 times the rate for substance-abuse—only clients and five times the rate for mental-disorder-only clients (Coffey et al. 2001). This estimate is based on an analysis of the CSAT/Center for Mental Health Services (CMHS) Integrated Data Base Project, in which a team studied information from the mental health, substance abuse, and Medicaid agencies in Delaware, Oklahoma, and Washington. Using a broad coding for health policy research to study discharges between 1990-1995 from community hospitals nationwide, Duffy (2004, p. 45) estimated that clients classified as having both a substance-related disorder and a mental disorder significantly “…increased from 9.4 to 17.22 per 10,000 population…” with the 35–45 year age group increasing the most among the 7 age groups studied from childhood to 65 or older.
Treatment Innovation for Other Populations With COD
Further treatment innovation has been required to meet the needs and associated problems of other treatment populations with high rates of COD such as people who are homeless, those in the criminal justice system, persons living with HIV/AIDS and other infectious diseases (e.g., hepatitis), and those with trauma and posttraumatic stress disorder (PTSD).
Homeless populations
Data on the increasing rates of co-occurring mental and substance use disorders in homeless populations are now available (North et al. 2004). North and colleagues estimate that rates of co-occurring Axis I and substance use disorders among females who are homeless increased from 14.3 percent in 1990 to 36.7 percent in 2000 and that rates among men who are homeless increased from 23.2 percent in 1990 to 32.2 percent in 2000.
North and colleagues also compared data collected in their 2000 study with estimates from ECA data collected in the early 1980s. They found that alcohol and drug use for both males and females rose considerably over the 2 decades. In 2000, 84 percent of the men who were homeless and 58 percent of the women who were homeless had a substance use disorder (North et al. 2004). The article reports an increase in bipolar disorder from 1990 to 2000 and an increase in major depression from 1980 to 2000. (Major depression accounted for the majority of all Axis I non-substance disorders.) The authors also noted that non-Axis I antisocial personality disorder (APD) appeared to change little from 1980 to 2000, with 10 to 20 percent of women who were homeless and 20 to 25 percent of men who were homeless receiving APD diagnoses in both time periods (North et al. 2004).
The increased prevalence of COD among people who are homeless and the need to provide services to this growing population has led to treatment innovations and research on service delivery. One of the main challenges is how to engage this group in treatment. CMHS’s Access to Community Care and Effective Services and Supports initiative, which supported programs in nine States over a 5-year period, indicated the effectiveness of integrated systems, including the value of street outreach (Lam and Rosenheck 1999; Rosenheck et al. 1998). Both systems integration and comprehensive services, such as Assertive Community Treatment (ACT) and Intensive Case Management (ICM), were seen as essential and effective (Integrating Systems of Care 1999; Winarski and Dubus 1994). (See chapter 6 for a discussion of these approaches.)
Offenders
The Bureau of Justice Statistics estimates that “at midyear 1998, an estimated 283,800 mentally ill offenders were incarcerated in the Nation’s prisons and jails” (Ditton 1999, p. 1). Surveys by the Bureau found that “16 percent of State prison inmates, 7 percent of Federal inmates, and 16 percent of those in local jails reported either a mental condition or an overnight stay in a mental hospital” (Ditton 1999). In addition, an estimated 547,800 probationers—16 percent—said they had had a mental condition or stayed overnight in a mental hospital at some point in their lifetime (Ditton 1999).
The Office of National Drug Control Policy (ONDCP) emphasized that “the fastest and most cost-effective way to reduce the demand for illicit drugs is to treat chronic, hard core drug users” (ONDCP 1995, p. 53). These “hard core users” are in need of COD services. The NTIES study reported that, when given the choice to rate their desire for certain services as “not important,” “somewhat important,” or “very important,” 37 percent of a population that was predominantly criminal-justice—involved rated mental health services as “very important” (Karageorge 2000).
The substance abuse treatment and mental health services communities have been called on to provide, or assist in providing, treatment to these individuals. This requires the integration of substance abuse treatment and mental health services and the combination of these approaches with those that address criminal thinking and behavior, while attending to both public health and public safety concerns.
HIV/AIDS and infectious diseases
The association between psychological dysfunction and a tendency to engage in high-risk behaviors (Joe et al. 1991; Simpson et al. 1993) suggests that it is important to integrate HIV/AIDS prevention and treatment with substance abuse treatment and mental health services for the COD population. Advances in the treatment of HIV/AIDS (such as antiretroviral combination therapy, including protease inhibitors) and the improved outcomes resulting from such therapies potentially will extend the survival of those with HIV/AIDS and co-occurring disorders. This will extend their requirement for continued mental health and substance abuse services. For persons with COD who also have HIV/AIDS or other infectious diseases (e.g., hepatitis C), primary medical care should be integrated with COD treatment. To be successful, this treatment should include an emphasis on treatment adherence (see chapter 7 for one such model).
Trauma and PTSD
Many persons with substance use disorders have experienced trauma, often as a result of abuse. A significant number of them have the recognized mental disorder known as PTSD. Recent studies have demonstrated strong connections between trauma and addictions, including the possibility that childhood abuse plays a part in the development of substance use disorders (Anderson et al. 2002; Brady et al. 2000; Chilcoat and Breslau 1998b ; Jacobsen et al. 2001). Although substance abuse treatment clinicians have counseled these clients for years, new treatment strategies for PTSD and trauma have expanded treatment options (see chapter 8 and appendix D). The forthcoming TIP Substance Abuse Treatment and Trauma will explore these issues in depth (CSAT in development d).
Changes in Treatment Delivery
The substance abuse treatment field has recognized the importance of COD programming. In 1995, only 37 percent of the substance use disorder treatment programs reporting data to the Substance Abuse and Mental Health Services Administration (SAMHSA) offered COD programming. By 1997, this percentage had increased to almost half (data not shown).
According to 2002 N-SSATS data, the number of programs for COD peaked in 1999, followed by a slight decline in 2000 that remained constant in 2002. This tracked the number of substance use disorder treatment providers, which also peaked in 1999. In 1999, there were 15,239 substance abuse treatment programs reporting to SAMHSA; in 2000, there were 13,428; in 2002, there were 13,720 (OAS 2003a ). Figure 1-3 shows that the number of programs for people with COD decreased slightly from 1999 to 2000, from 6,818 to 6,696, but remained constant in 2002 at 6,696 (OAS 2003a ). However, the ratio between the total number of substance abuse treatment programs and those offering COD programming has been relatively stable since 1997, increasing slightly from 44.7 percent in 1999 to 49.9 percent in 2000, and then remaining roughly constant at 48.8 percent in 2002.
An important consideration for the public mental health and substance abuse delivery systems is the recognition that not all people with emotional problems are candidates for care within the public mental health system. Because many States prioritize the funding of mental health slots by providing access to those who meet the criteria for the most severe and persistent mental illnesses, it is important for treatment providers to recognize the criteria that their State jurisdiction uses to provide care. For example, a treatment program may be aware that a person has psychological symptoms signifying stress, a diagnosable mental disorder, a serious mental disorder, a severe and persistent mental disorder, or, finally, a severe and persistent mental disorder with disability. From the point of view of the behavioral healthcare delivery system, these distinctions are important. In a State that restricts the use of its Federal community mental health services dollars to those with severe and persistent mental illness, a person not meeting the criteria for that condition may not be eligible for mental health services.
If a client/consumer has a primary substance abuse problem and a “non-eligible” mental disorder—that is, a disorder that cannot by regulation or law be treated in a public mental health program—then all providers should be aware of this. The difference between ideal care and available care is critical to the utility of this TIP. Furthermore, during periods of financial difficulty, the prospect of additional resources being created to address complex problems is not likely. Thus, an integrated care framework is preferred in this TIP. An integrated framework recognizes that quality evidence-based individualized care can be provided within a behavioral health delivery system using existing resources and partnerships.
Advances in Treatment
Advances in the treatment of COD, such as improved assessments, psychological interventions, psychiatric medications, and new models and methods, have greatly increased available options for the counselor and the client.
“No wrong door” policy
The publication of Changing the Conversation (CSAT 2000a ) signaled several fundamental advances in the field. Of particular importance is the principle of “no wrong door.” This principle has served to alert treatment providers that the healthcare delivery system, and each provider within it, has a responsibility to address the range of client needs wherever and whenever a client presents for care. When clients appear at a facility that is not qualified to provide some type of needed service, those clients should carefully be guided to appropriate, cooperating facilities, with followup by staff to ensure that clients receive proper care. The evolution of the Changing the Conversation paradigm signals a recognition that recovery is applicable to all people in need of substance abuse services: to the client with psychiatric problems in the substance abuse treatment delivery system, the client with substance abuse problems in the traditional mental health services delivery system, or the client with co-occurring behavior problems in a traditional physical health delivery system. Every “door” in the healthcare delivery system should be the “right” door.
Treatment approaches are emerging with demonstrated effectiveness in achieving positive outcomes for clients with COD.
Mutual self-help for people with COD
Based on the Alcoholics Anonymous model, the mutual self-help movement has grown to encompass a wide variety of addictions. Narcotics Anonymous and Cocaine Anonymous are two of the largest mutual self-help organizations for chemical addiction; Recoveries Anonymous and Schizophrenics Anonymous are the best known for mental illness. Though these typically are referred to as “self-help” groups, this TIP adopts the term “mutual self-help” because it is more descriptive of the way most participants see these groups—as a means of both helping themselves and supporting each other in achieving specific personal goals.
Mutual self-help programs, which include but are not limited to 12-Step groups, apply a broad spectrum of personal responsibility and peer support principles, usually including 12-Step methods that prescribe a planned regimen of change. In recent years, mutual self-help groups that have been adapted to clients with COD have become increasingly available. A more extensive discussion of these dual recovery mutual self-help programs can be found in chapter 7.
Integrated care as a priority for people with severe and persistent mental illness
For those with severe and persistent mental illness, integrated treatment, as originally articulated by Minkoff (1989), emphasized the correspondence between the treatment models for mental illness and addiction in a residential setting. The model stressed a parallel view of recovery, concomitant treatment of mental illness and substance abuse, application of treatment stages, and the use of strategies from both the mental health and substance abuse treatment fields. During the last decade, integrated treatment has continued to evolve, and several models have been described (Drake and Mueser 1996b ; Lehman and Dixon 1995; Minkoff and Drake 1991; Solomon et al. 1993).
For the purposes of this TIP, integrated treatment refers more broadly to any mechanism by which treatment interventions for COD are combined within the context of a primary treatment relationship or service setting. Integrated treatment is a means of coordinating substance abuse and mental health interventions to treat the whole person more effectively. In a review of mental health center-based research for clients with serious and persistent mental illness, Drake and colleagues (1998b ) concluded that comprehensive, integrated treatment, “especially when delivered for 18 months or longer, resulted in significant reductions of substance abuse and, in some cases, in substantial rates of remission, as well as reductions in hospital use and/or improvements in other outcomes” (p. 601). Several studies based in substance abuse treatment centers addressing a range of COD have demonstrated better treatment retention and outcome when mental health services were integrated onsite (Charney et al. 2001; McLellan et al. 1993; Saxon and Calsyn 1995; Weisner et al. 2001).
An integrated care framework supports the provision of some assessment and treatment wherever the client enters the treatment system, ensures that arrangements to facilitate consultations are in place to respond to client issues for which a provider does not have in-house expertise, and encourages all counselors and programs to develop increased competency in treating individuals with COD. Several States have received Community Action Grants from SAMHSA to develop comprehensive continuous integrated systems of care. It is especially important that appropriate substance abuse and mental health services for clients with COD be designed specifically for the substance abuse treatment system—a system that addresses a wide range of COD, not mainly those with severe and persistent mental illness. This subject is explored in chapter 3, and some approaches to integrated treatment in substance abuse treatment settings are examined in chapter 3 and chapter 6.
Development of effective approaches, models, and strategies
Treatment approaches are emerging with demonstrated effectiveness in achieving positive outcomes for clients with COD. These include a variety of promising treatment approaches that provide comprehensive integrated treatment. Successful strategies with important implications for clients with COD also include interventions based on addiction work in contingency management, cognitive—behavioral therapy, relapse prevention, and motivational interviewing. These strategies are discussed in chapter 5. In fact, it is now possible to identify “guiding principles” and “fundamental elements” for COD treatment in COD settings that are common to a variety of approaches. These are discussed at length in chapter 3 and chapter 6, respectively. Specific program models that have proven effective for the COD population with serious mental illness include ACT and the Modified Therapeutic Community. ICM also has proven useful in treating clients with COD. See chapter 6 for a discussion of these models.
Pharmacological advances
Pharmacological advances over the past decade have produced antipsychotic, antidepressant, anticonvulsant, and other medications with greater effectiveness and fewer side effects (see appendix F for a listing of medications). With the support available from better medication regimens, many people who once would have been too unstable for substance abuse treatment, or institutionalized with a poor prognosis, have been able to lead more functional lives. To meet the needs of this population, the substance abuse treatment counselor needs both greater understanding of the signs and symptoms of mental illness and greater capacity for consultation with trained mental healthcare providers. As substance abuse treatment counselors learn more about mental illness, they are better able to partner with mental health counselors to design effective treatment for both types of disorders. Such partnerships benefit mental health agencies as well, helping them enhance their ability to treat clients with substance abuse issues.
Increasingly, substance abuse treatment counselors and programs have come to appreciate the importance of providing medication to control symptoms as an essential part of treatment. The counselor has an important role in describing client behavior and symptoms to ensure that proper medication is prescribed when needed. The peer community also is a powerful tool that can be employed to support and monitor medication adherence. Support from mutual self-help groups can include learning about the effects of medication and learning to accept medication as part of recovery. Monitoring involves clients learning from and reflecting on their own and others’ reactions, thoughts, and feelings about the ways medications affect them, both positively as symptoms are alleviated, and negatively as unwanted side effects may occur.
Some Recent Developments
Since the consensus panel for this TIP was convened, there have been several important developments in the field of co-occurring disorders. Following is a description of the most recent developments in the field.
National Registry of Effective Programs and Practices
To help its practice and policymaking constituents learn more about evidence-based programs, SAMHSA’s Center for Substance Abuse Prevention created the National Registry of Effective Programs and Practices (NREPP), a resource to review and identify effective programs derived primarily from existing scientific literature, effective programs assessed by other rating processes, SAMHSA, and solicitations to the field. When co-occurring disorder treatment programs are submitted for NREPP consideration, teams of scientists review the programs based on four criteria: (1) co-occurring disorders programs, (2) psychopharmacological programs, (3) workplace programs, and (4) general substance abuse prevention and treatment programs. Evaluation is based on methodological quality (a program’s overall rigor and substantive contribution) and appropriateness (dissemination capability, cultural sensitivity, and consumer involvement to inform a total rating that describes a program’s readiness for adoption and replication). Programs that demonstrate a commitment to complete assessment and comprehensive services receive priority. For programs that target persons with serious mental disorders, priority is given to approaches that integrate substance abuse treatment and mental health services. Targeted techniques and strategies are also eligible for NREPP review. For more detailed information about NREPP, see www.modelprograms.samhsa.gov.
Co-Occurring Disorders State Incentive Grants
The Co-Occurring Disorders State Incentive Grants (COSIG) (funded through SAMHSA’s CSAT and CMHS) provide funding to the States to develop or enhance their infrastructure to increase their capacity to provide accessible, effective, comprehensive, coordinated/integrated, and evidence-based treatment services to persons with COD. COSIG uses the definition of co-occurring disorders from this TIP (see the beginning of this chapter). It supports infrastructure development and services across the continuum of COD, from least severe to most severe, but the emphasis is on people with less severe mental disorders and more severe substance use disorders, and on people with more severe mental disorders and less severe substance use disorders (i.e., quadrants II and III—see chapter 2 for a description of the four quadrants). COSIG is appropriate for States at any level of infrastructure development. COSIG also provides an opportunity to evaluate the feasibility, validity, and reliability of the proposed co-occurring performance measures for the future Performance Partnership Grants. Some States and communities throughout the country already have initiated system-level changes and developed innovative programs that overcome barriers to providing services for individuals of all ages who have COD. The COSIG program reflects the experience of States to date. For more information, see www.samhsa.gov.
Co-Occurring Center for Excellence
As a result of the pressing need to disseminate and support the adoption of evidence- and consensus-based practices in the field of COD, SAMHSA established the Co-Occurring Center for Excellence (COCE) in 2003. COCE provides SAMHSA and the field with key resources needed to disseminate knowledge and increase adoption of evidence-based practices in the systems and programs that serve people with COD. The COCE mission is to
-
Transmit advances in substance abuse and mental health treatment that address all levels of mental disorder severity and that can be adapted to the unique needs of each client.
-
Guide enhancements in the infrastructure and clinical capacities of the substance abuse and mental health service systems.
-
Foster the infusion and adoption of evidence-based treatment and program innovation into clinical practice.
To guide its work, COCE has developed a framework that locates the key topics in COD along three dimensions: services and service systems, infrastructure, and special populations. Services and service systems include providers and the services they offer; the nature and structure of the organizations and systems in which services are delivered; and the interrelationships among various providers, organizations, and systems. Infrastructure includes the wide variety of national, State, and local policies, programs, and resources that support, facilitate, catalyze, and otherwise contribute to the work of service providers and service systems. Special populations identifies groups who may require special services, settings, or accommodations to reap the full benefit of COD-related services. At this time, the core products and services of the COCE are envisioned as technical assistance and training, a Web site, (www.coce.samhsa.gov),meetings and conferences, and future COCE products and services.
Report to Congress on the Prevention and Treatment of Co-Occurring Substance Use Disorders and Mental Disorders
In response to a Congressional mandate, in December 2002 the Department of Health and Human Services provided Congress with a comprehensive report on treatment and prevention of co-occurring substance abuse and mental disorders. The report emphasizes that people with co-occurring disorders can and do recover with appropriate treatment and support services. It also finds there are many longstanding systemic barriers to appropriate treatment and support services for people with co-occurring disorders, including separate administrative structures, eligibility criteria, and funding streams, as well as limited resources for both mental health services and substance abuse treatment. The report identifies the need for various Federal and State agencies, providers, researchers, recovering persons, families, and others to work together to create a system in which both disorders are addressed as primary and treated as such. It also outlines a 5-year blueprint for action to improve the opportunity for recovery by increasing the availability of quality prevention, diagnosis, and treatment services for people with co-occurring disorders. To access the full report, see www.samhsa.gov/reports/congress2002/index.html.
As substance abuse treatment counselors learn more about mental illness, they can better partner with mental health counselors to design effective treatment for both disorders.
Co-Occurring Disorders: Integrated Dual Disorders Treatment Implementation Resource Kit
Known simply as the “tool kit,” and developed by the Psychiatric Research Center at New Hampshire-Dartmouth under the leadership of Robert E. Drake, M.D., Ph.D., this resource package specifically targets clients with COD who have SMI and who are seeking care through mental health services available in their community. The six evidence-based practices described in the tool kit are collaborative psychopharmacology, ACT, family psychoeducation, supported employment, illness management and recovery, and integrated dual disorders treatment (substance use and mental illness). Using materials germane to a variety of audiences (i.e., consumers, family members/caregivers, mental health program leaders, public mental health authorities, and practitioners/clinical supervisors), the tool kit articulates a flexible basic plan that allows materials to be used to implement best practices to their maximum effect. The tool kit is being produced under a contract with SAMHSA’s CMHS and through a grant from The Robert Wood Johnson Foundation (CMHS in development).
The TIP is structured to meet the needs of the addiction counselor with a basic background as well as the differing needs of those with intermediate and advanced backgrounds.
Organization of This TIP
Scope
The TIP attempts to summarize for the clinician the state-of-the-art in the treatment of COD in the substance abuse and mental health fields. It contains chapters on terminology, assessment, and treatment strategies and models, as well as recommendations for treatment, research, and policy planning.
The primary concern of this TIP is co-occurring substance use (abuse and dependence) and mental disorders, even though it is recognized that this same vulnerable population also is subject to many other physical and social ills. The TIP includes important work on nicotine dependence, a somewhat large and separate body of work that admittedly does need further integration into the general field of COD. Nicotine dependency is treated here as an important cross-cutting issue. Finally, although the TIP does address several specific populations (i.e., homeless, criminal justice, and women), it does this briefly and does not describe programs specifically for adolescents or for such specialized populations as new Asian and Hispanic/Latino immigrants. At the same time, the authors fully recognize, and the TIP states, that all COD treatment must be culturally relevant.
Audience
The primary audience for this TIP is substance abuse treatment clinicians and counselors, many, but not all, of whom possess certification in substance abuse counseling or related professional licensing. Some may have credentials in the treatment of mental disorders or in criminal justice services. The TIP is structured to meet the needs of the addiction counselor with a basic background as well as the differing needs of those with intermediate and advanced backgrounds. Another equally important audience for the TIP is mental health staff. Secondary audiences include educators, researchers, primary care providers, criminal justice staff, and other healthcare and social service personnel who work with people with COD.
Approach
The TIP uses three criteria for inclusion of a particular strategy, technique, or model: (1) definitive research (i.e., evidence-based treatments), (2) well-articulated approaches with empirical support, and (3) consensus panel agreement about established clinical practice. The information in this TIP derives from a variety of sources, including the research literature, conceptual writings, descriptions of established program models, accumulated clinical experience and expertise, government reports, and other available empirical evidence. It is a document that reflects the current state of clinical wisdom in the treatment of clients with COD.
The TIP keeps two questions in the forefront:
-
What does the clinician need to know?
-
How can the information be conveyed in a manner that makes it readily accessible?
Guidance for the Reader
This TIP is both a resource document and a guide on COD that contains both up-to-date knowledge and instructive material. It includes selected literature reviews, synopses of many COD treatment approaches, and some empirical information. The scope of the work in this field generated a complex and extensive document that is probably best read by chapter or section. It contains text boxes, case histories, illustrations, and summaries to synthesize knowledge that is grounded in the practical realities of clinical cases and real situations. A special feature throughout the TIP—“Advice to the Counselor”—provides the TIP’s most direct and accessible guidance for the counselor. Readers with basic backgrounds, such as addiction counselors or other practitioners, can study the Advice to the Counselor boxes first for the most immediate practical guidance. In particular, the Advice to the Counselor boxes provide a distillation of what the counselor needs to know and what steps to take, which can be followed by a more detailed reading of the relevant material in the section or chapter.
The chair and co-chair of the TIP consensus panel plan to continue working with providers and treatment agencies, and encouraging others to do likewise, to translate the concepts and methods of the TIP into other useable tools specifically shaped to the needs and resources of each agency and situation. It is the hope of the consensus panel that the reader will come away with increased knowledge, encouragement, and resources for the important work of treating persons with COD.
Organization
The TIP is organized into 9 chapters and 14 appendices. Subject areas addressed in each of the remaining chapters and appendices are as follows:
Chapter 2. Definitions, terms, and classification systems for co-occurring disorders
This chapter reviews terminology and classifications related to substance use, clients, treatment, programs, and systems for clients with COD. Key terms used in the TIP and in the field are defined to help the reader understand the framework and language used in this TIP and how this language relates to other terminology and classifications that are familiar to the reader. The main classification systems currently in use in the field are presented.
Chapter 3. Keys to successful programming
The chapter begins with a review of some guiding principles in treatment of clients with COD, and key challenges to establishing services in substance abuse treatment settings are highlighted. This section also presents a system for classifying substance abuse treatment programs to determine an appropriate level of services and care. The chapter describes some service delivery issues including access, assessment, integrated treatment, comprehensive services, and continuity of care. Finally, critical issues in workforce development are discussed, including values, competencies, education, and training.
Chapter 4. Assessment
This chapter reviews the key principles of assessment, selected assessment instruments, and the assessment process. The chapter also addresses the specific relationship of assessment to treatment planning.
Chapter 5. Strategies for working with clients with co-occurring disorders
This chapter presents guidelines for developing a successful therapeutic relationship with individuals who have COD. It describes specific techniques for counselors that appear to be the most successful in treating clients with COD and introduces guidelines that are important for the successful use of all these strategies.
Chapter 6. Traditional settings and models
The chapter begins by addressing essential programming for clients with COD that can readily be offered in most substance abuse treatment settings. Overarching considerations in effective treatment for this population, regardless of setting, are reviewed. Practices are highlighted that have proven effective for the treatment of persons with COD in outpatient and residential settings. The chapter also highlights several distinctive models.
Chapter 7. Special settings and specific populations
This chapter addresses issues related to providing treatment to clients with COD in acute care and other medical settings, as well as the need to sustain these programs. Because of the critical role mutual self-help groups play in recovery, several dual recovery mutual self-help groups that address the specific concerns of clients with COD are described. Resources available through advocacy groups are highlighted. Finally, the chapter discusses the need to address the particular needs of people with COD within three key populations: homeless persons, criminal justice populations, and women.
Chapter 8. A brief overview of specific mental disorders and cross-cutting issues
With the permission of American Psychiatric Publishing, Inc. (APPI), the consensus panel has taken the opportunity to present to the substance abuse treatment audience basic information contained in the Diagnostic and Statistical Manual for Mental Disorders, 4th edition, Text Revised (DSM-IV-TR). The chapter updates material that was presented on the major disorders covered in TIP 9 (i.e., personality disorders, mood disorders, anxiety disorders, and psychotic disorders) and adds other mental disorders with particular relevance to COD that were not covered in TIP 9 (i.e., attention deficit/hyperactivity disorder, PTSD, eating disorders, and pathological gambling). Suicidality and nicotine dependency are presented as cross-cutting issues. The consensus panel is pleased that APPI has allowed this liberal use of its materials to help foster the co-occurring disorders field and positive interchange between the substance abuse treatment and mental health services fields.
The chapter contains key information about substance abuse and the particular mental disorder, highlighting advice to the counselor to help in working with clients with those disorders. A relevant case history accompanies each disorder in this chapter. This chapter is meant to function as a “quick reference” to help the substance abuse treatment counselor understand the mental disorder diagnosis and its implications for treatment planning. Appendix D contains a more extensive discussion of the same disorders.
Chapter 9. Substance-induced disorders
This chapter provides information on mental disorder symptoms caused by the use of substances. It outlines the toxic effect of substances and provides an overview of substance-induced symptoms that can mimic mental disorders.
Appendices
Appendix A. Bibliography
Appendix A contains the references cited in this TIP and other resources used for background purposes but not specifically cited.
Appendix B. Acronyms
Appendix B contains a key to all the acronyms used in this TIP.
Appendix C. Glossary of terms
This appendix contains the definitions of terms used in this TIP, with the exception of terminology related to specific mental disorders discussed in chapter 8 and appendix D. For these specialized terms, the reader is advised to consult a medical dictionary.
Appendix D. Specific mental disorders: Additional guidance for the counselor
Clients with COD entering treatment often have several disorders, each of which is associated with a growing body of knowledge and range of treatment options. This appendix is meant to serve substance abuse treatment counselors and programs as a resource and training document that provides more extensive information on individual mental disorders than could be included in chapter 8. Although most readers will not read the entire appendix at one time, this mental disorder-oriented section is included so that a counselor who is working with a new client with one or more of these disorders can have detailed information readily available.
Appendix E. Emerging models
In this appendix, the reader can find descriptions of several recent models of care for persons with COD that were (or are being) evaluated under initiatives funded by SAMHSA’s CSAT. Though selective and based primarily on available information from recent SAMHSA initiatives, it is hoped that these models will suggest ways in which readers working with a variety of client types and symptom severities in different settings can improve their capacities to assess and treat these clients.
Appendix F. Common medications for disorders
Because medication is such an important adjunct to treatment, this appendix offers a brief review of key issues in pharmacologic management. A table of common medications for various disorders follows this discussion, with comments on the effects of these medications and their implications for addiction counselors and treatment. This material is taken from the Pharmacological Management section of TIP 9 (CSAT 1994a , pp. 91–94), followed by the complete text of Psychotherapeutic Medications 2004: What Every Counselor Should Know (Mid-America Addiction Technology Transfer Center 2004).
Appendix G. Screening and assessment instruments
A list of selected screening and assessment tools referenced in chapter 4, along with key information on the use of each instrument, appears in this appendix. As a full review of these instruments was beyond the scope of this TIP, readers are urged to review the literature to determine their reliability, validity, and utility, and to gain an understanding of their applicability to specific situations.
Appendix H. Sample screening instruments
This appendix offers two screening instruments available for unrestricted use:
-
The Mental Health Screening Form-III
-
The Simple Screening Instrument for Substance Abuse
Appendix I. Selected resources of training
Here the reader finds some of the most readily available and well-used sources of training in substance abuse treatment, mental health services, and co-occurring disorders.
Appendix J. Dual recovery mutual self-help programs and other resources for consumers and providers
This appendix provides a brief description and contact information for several mutual self-help groups discussed in the TIP.
Appendix K. Confidentiality
This appendix provides a brief description of the Federal Alcohol and Drug Confidentiality Law and Regulations (42 C.F.R. Part 2) and the Health Insurance Portability and Accountability Act of 1996.
Figures
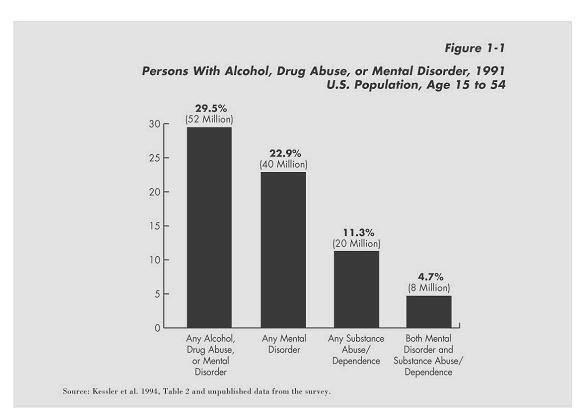
Figure 1-1. Persons With Alcohol, Drug Abuse, or Mental Disorder in the Past Year (see Endnote i )
- i
-
“These estimates are from the National Comorbidity Survey. The survey was based on interviews administered to a probability sample of the noninstitutionalized U.S. civilian population. The NCS sample consisted of 8,098 respondents, age 15 to 54 years. This survey was conducted from September 1990 to February 1992. DSM-III-R criteria were used as the basis for assessing disorders in the general population. A random sample of initial nonrespondents was contacted further and received a financial incentive to participate. A nonresponse weight was used to adjust for the higher rates of [alcohol, drugs, or mental (ADM) disorders] found in the sample of initial nonresponders. The Composite International Diagnostic Interview was modified to eliminate rare diagnoses in the age group studied and to add probes to improve understanding and motivation. The ‘substance abuse/dependence’ category includes drugs and alcohol. ‘Any ADM disorder’ includes the following: affective, anxiety, substance abuse/dependence, nonaffective psychosis, and antisocial personality disorders. ‘Affective disorders’ include major depressive episode, manic episode, and dysthymia. Anxiety disorders include panic disorder, agoraphobia, social phobia, simple phobia, and generalized anxiety disorder. Antisocial personality was assessed only on a lifetime basis. Nonaffective psychoses include schizophrenias, delusional disorder, and atypical psychoses. Substance abuse/dependence includes both abuse of and dependence on alcohol and other drugs” (SAMHSA 1998, p. 7).)
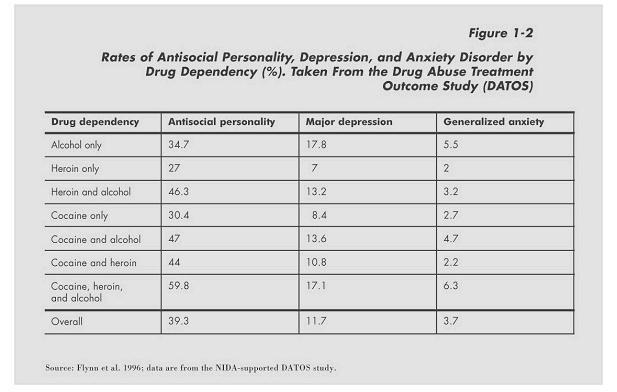
Figure 1-2. Rates of Antisocial Personality, Depression, and Anxiety Disorder by Drug Dependency