In This Chapter…
- Screening and Basic Assessment for COD
- The Assessment Process
Overview
This chapter consists of three parts: (1) an overview of the basic screening and assessment approach that should be a part of any program for clients with co-occurring disorders (COD); (2) an outline of the 12 steps to an ideal assessment, including some instruments that can be used in assessing COD; and (3) a discussion of key considerations in treatment matching.
Ideally, information needs to be collected continuously, and assessments revised and monitored as the client moves through recovery. A comprehensive assessment as described in the main section of this chapter leads to improved treatment planning, and it is the intent of this chapter to provide a model of optimal process of evaluation for clients with COD and to encourage the field to move toward this ideal. Nonetheless, the panel recognizes that not all agencies and providers have the resources to conduct immediate and thorough screenings. Therefore, the chapter provides a description of the initial screening and the basic or minimal assessment of COD necessary for the initial treatment planning.
A basic assessment covers the key information required for treatment matching and treatment planning. Specifically, the basic assessment offers a structure with which to obtain
- Basic demographic and historical information, and identification of established or probable diagnoses and associated impairments
- General strengths and problem areas
- Stage of change or stage of treatment for both substance abuse and mental health problems
- Preliminary determination of the severity of the COD as a guide to final level of care determination
Note that medical issues (including physical disability and sexually transmitted diseases), cultural issues, gender-specific and sexual orientation issues, and legal issues always must be addressed, whether basic or more comprehensive assessment is performed. The consensus panel assumes that appropriate procedures are in place to address these and other important issues that must be included in treatment planning. However, the focus of this chapter, in keeping with the purpose of this TIP, is on screening and assessment related to COD.
Screening and Basic Assessment for COD
This section provides an overview of the screening and assessment process for COD. In carrying out these processes, counselors should understand the limitations of their licensure or certification authority to diagnose or assess mental disorders. Generally, however, collecting assessment information is a legitimate and legal activity even for unlicensed providers, provided that they do not use diagnostic labels as conclusions or opinions about the client. Information gathered in this way is needed to ensure the client is placed in the most appropriate treatment setting (as discussed later in this chapter) and to assist in providing mental disorder care that addresses each disorder.
In addition, there are a number of circumstances that can affect validity and test responses that may not be obvious to the beginning counselor, such as the manner in which instructions are given to the client, the setting where the screening or assessment takes place, privacy (or the lack thereof), and trust and rapport between the client and counselor. Throughout the process it is important to be sensitive to cultural context and to the different presentations of both substance use and mental disorders that may occur in various cultures.
The following Advice to the Counselor section gives an overview of the basic “do’s and don’ts” for assessing for COD. Detailed discussions of these important screening/assessment and cultural issues are beyond the scope of this TIP. For more information on basic screening and assessment information, see chapters 4 and 5 in Evans and Sullivan (2001), National Institute on Drug Abuse (NIDA) (1994), and the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (Allen and Wilson 2003). For information on cultural issues, see the forthcoming TIP Improving Cultural Competence in Substance Abuse Treatment (Center for Substance Abuse Treatment [CSAT] in development a).
Screening
Screening is a formal process of testing to determine whether a client does or does not warrant further attention at the current time in regard to a particular disorder and, in this context, the possibility of a co-occurring substance use or mental disorder. The screening process for COD seeks to answer a “yes” or “no” question: Does the substance abuse (or mental health) client being screened show signs of a possible mental health (or substance abuse) problem? Note that the screening process does not necessarily identify what kind of problem the person might have or how serious it might be, but determines whether or not further assessment is warranted. A screening process can be designed so that it can be conducted by counselors using their basic counseling skills. There are seldom any legal or professional restraints on who can be trained to conduct a screening.
Screening processes always should define a protocol for determining which clients screen positive and for ensuring that those clients receive a thorough assessment. That is, a professionally designed screening process establishes precisely how any screening tools or questions are to be scored and indicates what constitutes scoring positive for a particular possible problem (often called “establishing cut-off scores”). Additionally, the screening protocol details exactly what takes place after a client scores in the positive range and provides the necessary standard forms to be used to document both the results of all later assessments and that each staff member has carried out his or her responsibilities in the process.
So, what can a substance abuse treatment counselor do in terms of screening? All counselors can be trained to screen for COD. This screening often entails having a client respond to a specific set of questions, scoring those questions according to how the counselor was trained, and then taking the next “yes” or “no” step in the process depending on the results and the design of the screening process. In substance abuse treatment or mental health service settings, every counselor or clinician who conducts intake or assessment should be able to screen for the most common COD and know how to implement the protocol for obtaining COD assessment information and recommendations. For substance abuse treatment agencies that are instituting a mental health screening process, appendix H reproduces the Mental Health Screening Form-III (Carroll and McGinley 2001). This instrument is intended for use as a rough screening device for clients seeking admission to substance abuse treatment programs. (Note that while the consensus panel believes that this instrument is useful, it has received limited validation [Carroll and McGinley 2001].)
Advice to the Counselor:
Do’s and Don’ts of Assessment for COD
- Do keep in mind that assessment is about getting to know a person with complex and individual needs. Do not rely on tools alone for a comprehensive assessment.
- Do always make every effort to contact all involved parties, including family members, persons who have treated the client previously, other mental health and substance abuse treatment providers, friends, significant others, probation officers as quickly as possible in the assessment process. (These other sources of information will henceforth be referred to as collaterals.)
- Don’t allow preconceptions about addiction to interfere with learning about what the client really needs (e.g., “All mental symptoms tend to be caused by addiction unless proven otherwise”). Co-occurring disorders are as likely to be underrecognized as overrecognized. Assume initially that an established diagnosis and treatment regime for mental illness is correct, and advise clients to continue with those recommendations until careful reevaluation has taken place.
- Do become familiar with the diagnostic criteria for common mental disorders, including personality disorders, and with the names and indications of common psychiatric medications. Also become familiar with the criteria in your own State for determining who is a mental health priority client. Know the process for referring clients for mental health case management services or for collaborating with mental health treatment providers.
- Don’t assume that there is one correct treatment approach or program for any type of COD. The purpose of assessment is to collect information about multiple variables that will permit individualized treatment matching. It is particularly important to assess stage of change for each problem and the client’s level of ability to follow treatment recommendations.
- Do become familiar with the specific role that your program or setting plays in delivering services related to COD in the wider context of the system of care. This allows you to have a clearer idea of what clients your program will best serve and helps you to facilitate access to other settings for clients who might be better served elsewhere.
- Don’t be afraid to admit when you don’t know, either to the client or yourself. If you do not understand what is going on with a client, acknowledge that to the client, indicate that you will work with the client to find the answers, and then ask for help. Identify at least one supervisor who is knowledgeable about COD as a resource for asking questions.
- Most important, do remember that empathy and hope are the most valuable components of your work with a client. When in doubt about how to manage a client with COD, stay connected, be empathic and hopeful, and work with the client and the treatment team to try to figure out the best approach over time.
Basic Assessment
While both screening and assessment are ways of gathering information about the client in order to better treat him, assessment differs from screening in the following way:
- Screening is a process for evaluating the possible presence of a particular problem.
- Assessment is a process for defining the nature of that problem and developing specific treatment recommendations for addressing the problem.
A basic assessment consists of gathering key information and engaging in a process with the client that enables the counselor to understand the client’s readiness for change, problem areas, COD diagnosis(es), disabilities, and strengths. An assessment typically involves a clinical examination of the functioning and well-being of the client and includes a number of tests and written and oral exercises. The COD diagnosis is established by referral to a psychiatrist, clinical psychologist, or other qualified healthcare professional. Assessment of the client with COD is an ongoing process that should be repeated over time to capture the changing nature of the client’s status. Intake information consists of
- Background—family, trauma history, history of domestic violence (either as a batterer or as a battered person), marital status, legal involvement and financial situation, health, education, housing status, strengths and resources, and employment
- Substance use—age of first use, primary drugs used (including alcohol, patterns of drug use, and treatment episodes), and family history of substance use problems
- Mental health problems—family history of mental health problems, client history of mental health problems including diagnosis, hospitalization and other treatment, current symptoms and mental status, medications, and medication adherence
In addition, the basic information can be augmented by some objective measurement, such as that provided in the University of Rhode Island Change Assessment Scale (URICA) (McConnaughy et al. 1983), Addiction Severity Index (ASI) (McLellan et al. 1992), the Mental Health Screening Form-III (Carroll and McGinley 2001), and the Symptom Distress Scale (SDS) (McCorkle and Young 1978) (see appendices G and H for further information on selected instruments). It is essential for treatment planning that the counselor organize the collected information in a way that helps identify established mental disorder diagnoses and current treatment. The text box on page 71 highlights the role of instruments in the assessment process.
Careful attention to the characteristics of past episodes of substance abuse and abstinence with regard to mental health symptoms, impairments, diagnoses, and treatments can illuminate the role of substance abuse in maintaining, worsening, and/or interfering with the treatment of any mental disorder. Understanding a client’s mental health symptoms and impairments that persist during periods of abstinence of 30 days or more can be useful, particularly in understanding what the client copes with even when the acute effects of substance use are not present. For any period of abstinence that lasts a month or longer, the counselor can ask the client about mental health treatment and/or substance abuse treatment—what seemed to work, what did the client like or dislike, and why? On the other hand, if mental health symptoms (even suicidality or hallucinations) resolve in less than 30 days with abstinence from substances, then these symptoms are most likely substance induced and the best treatment is maintaining abstinence from substances.
The counselor also can ask what the mental health “ups and downs” are like for the client. That is, what is it like for the client when he or she gets worse (or “destabilizes”)? What—in detail—has happened in the past? And, what about getting better (“stabilizing”)—how does the client usually experience that? Clinician and client together should try to understand the specific effects that substances have had on that individual’s mental health symptoms, including the possible triggering of psychiatric symptoms by substance use. Clinicians also should attempt to document the diagnosis of a mental disorder, when it has been established, and determine diagnosis through referral when it has not been established. The consensus panel notes that many, if not most, individuals with COD have well-established diagnoses when they enter substance abuse treatment and encourages counselors to find out about any known diagnoses.
Treatment Planning
A comprehensive assessment serves as the basis for an individualized treatment plan. Appropriate treatment plans and treatment interventions can be quite complex, depending on what might be discovered in each domain. This leads to another fundamental principle:
- There is no single, correct intervention or program for individuals with COD. Rather, the appropriate treatment plan must be matched to individual needs according to these multiple considerations.
The following three cases illustrate how the above factors help to generate an integrated treatment plan that is appropriate to the needs and situation of a particular client.
Case 1: Maria M.
The client is a 38-year-old Hispanic/Latina woman who is the mother of two teenagers. Maria M. presents with an 11-year history of cocaine dependence, a 2-year history of opioid dependence, and a history of trauma related to a longstanding abusive relationship (now over for 6 years). She is not in an intimate relationship at present and there is no current indication that she is at risk for either violence or self-harm. She also has persistent major depression and panic treated with antidepressants. She is very motivated to receive treatment.
- Ideal Integrated Treatment Plan: The plan for Maria M. might include medication-assisted treatment (e.g., methadone or buprenorphine), continued antidepressant medication, 12-Step program attendance, and other recovery group support for cocaine dependence. She also could be referred to a group for trauma survivors that is designed specifically to help reduce symptoms of trauma and resolve long-term issues.
The Role of Assessment Tools
A frequent question asked by clinicians is
- What is the best (most valuable) assessment tool for COD?
The answer is
- There is no single gold standard assessment tool for COD. Many traditional clinical tools have a narrow focus on a specific problem, such as the Beck Depression Inventory (BDI) (Beck and Steer 1987), a list of 21 questions about mood and other symptoms of feeling depressed. Other tools have a broader focus and serve to organize a range of information so that the collection of such information is done in a standard, regular way by all counselors. The ASI, which is not a comprehensive assessment tool but a measure of addiction severity in multiple problem domains, is an example of this type of tool (McLellan et al. 1992). Not only does a tool such as the ASI help a counselor, through repetition, become adept at collecting the information, it also helps the counselor refine his or her sense of similarities and differences among clients. A standard mental status examination can serve a similar function for collecting information on current mental health symptoms. Despite the fact that there are some very good tools, no one tool is the equivalent of a comprehensive clinical assessment.
Individual, group, and family interventions could be coordinated by the primary counselor from opioid maintenance treatment. The focus of these interventions might be on relapse prevention skills, taking medication as prescribed, and identifying and managing trauma-related symptoms without using. An appropriate long-term goal would be to establish abstinence and engage Maria in longer-term psychotherapeutic interventions to reduce trauma symptoms and help resolve trauma issues. On the other hand, if a local mental health center had a psychiatrist trained and licensed to provide Suboxone (the combination of buprenorphine and nalaxone), her case could be based in the mental health center.
Case 2: George T.
The client is a 34-year-old married, employed African-American man with cocaine dependence, alcohol abuse, and bipolar disorder (stabilized on lithium) who is mandated to cocaine treatment by his employer due to a failed drug test. George T. and his family acknowledge that he needs help not to use cocaine but do not agree that alcohol is a significant problem (nor does his employer). He complains that his mood swings intensify when he is using cocaine.
- Ideal Integrated Treatment Plan: The ideal plan for this man might include participation in outpatient addiction treatment, plus continued provision of mood-stabilizing medication. In addition, he should be encouraged to attend a recovery group such as Cocaine Anonymous or Narcotics Anonymous. The addiction counselor would provide individual, group, and family interventions. The focus might be on gaining the skills and strategies required to handle cocaine cravings and to maintain abstinence from cocaine, as well as the skills needed to manage mood swings without using substances. Motivational counseling regarding alcohol and assistance in maintaining medication (lithium) adherence also could be part of the plan.
Case 3: Jane B.
The client is a 28-year-old single Caucasian female with a diagnosis of paranoid schizophrenia, alcohol dependence, crack cocaine dependence, and a history of multiple episodes of sexual victimization. Jane B. is homeless (living in a shelter), actively psychotic, and refuses to admit to a drug or alcohol problem. She has made frequent visits to the local emergency room for both mental health and medical complaints, but refuses any followup treatment. Her main requests are for money and food, not treatment. Jane has been offered involvement in a housing program that does not require treatment engagement or sobriety but has refused due to paranoia regarding working with staff to help her in this setting. Jane B. refuses all medication due to her paranoia, but does not appear to be acutely dangerous to herself or others.
- Ideal Integrated Treatment Plan: The plan for Jane B. might include an integrated case management team that is either based in the shelter or in a mental health service setting. The team would apply a range of engagement, motivational, and positive behavioral change strategies aimed at slowly developing a trusting relationship with this woman. Engagement would be promoted by providing assistance to Jane B. in obtaining food and disability benefits, and using those connections to help her engage gradually in treatment for either mental disorders or addiction—possibly by an initial offer of help in obtaining safe and stable housing. Peer support from other women also might be of value in promoting
her sense of safety and engagement.
All of these cases are appropriate examples of integrated treatment. The purpose of the assessment process is to develop a method for gathering information in an organized manner that allows the clinician to develop an appropriate treatment plan or recommendation. The remainder of this chapter will discuss how this assessment process might occur, and how the information gathered leads to a rational process of treatment planning. In Step 12 of the assessment process, readers will find an expanded treatment plan for the three clients discussed above.
The Assessment Process
This chapter is organized around 12 specific steps in the assessment process. Through these steps, the counselor seeks to accomplish the following aims:
- To obtain a more detailed chronological history of past mental symptoms, diagnosis, treatment, and impairment, particularly before the onset of substance abuse, and during periods of extended abstinence.
- To obtain a more detailed description of current strengths, supports, limitations, skill deficits, and cultural barriers related to following the recommended treatment regimen for any disorder or problem.
- To determine stage of change for each problem, and identify external contingencies that might help to promote treatment adherence.
Note that although the steps appear sequential, in fact some of them could occur simultaneously or in a different order, depending on the situation. It is particularly important to identify and attend to any acute safety needs, which often have to be addressed before a more comprehensive assessment process can occur. Sometimes, however, components of the assessment process are essential to address the client’s specific safety needs. For example, if a person is homeless, more information on that person’s mental status, resources, and overall situation is required to address that priority appropriately. Finally, it must be recognized that while the assessment seeks to identify individual needs and vulnerabilities as quickly as possible to initiate appropriate treatment, assessment is an ongoing process: As treatment proceeds and as other changes occur in the client’s life and mental status, counselors must actively seek current information rather than proceed on assumptions that might be no longer valid.
In the following discussion, validated assessment tools that are available to assist in this process are discussed with regard to their utility for counselors. There are a number of tools that are required by various States for use in their addiction systems (e.g., ASI [McLellan et al. 1992], American Society of Addiction Medicine (ASAM) Patient Placement Criteria [ASAM PPC-2R]). Particular attention will be given to the role of these tools in the COD assessment process, suggesting strategies to reduce duplication of effort where possible. It is beyond the scope of this TIP to provide detailed instructions for administering the tools mentioned in this TIP (with the exceptions of the Mental Health Screening Form-III [MHSF-III] and the Simple Screening Instrument for Substance Abuse [SSI-SA] in appendix H). Basic information about each instrument is given in appendix G, and readers can obtain more detailed information regarding administration and interpretation from the sources given for obtaining these instruments.
As a final point, this discussion primarily is directed toward substance abuse treatment clinicians working in substance abuse treatment settings, though many of the steps apply equally well to mental health clinicians in mental health settings. At certain key points in the discussion, particular information relevant to mental health clinicians is identified and described.
Assessment Step 1: Engage the Client
The first step in the assessment process is to engage the client in an empathic, welcoming manner and build a rapport to facilitate open disclosure of information regarding mental health problems, substance use disorders, and related issues. The aim is to create a safe and nonjudgmental environment in which sensitive personal issues may be discussed. Counselors should recognize that cultural issues, including the use of the client’s preferred language, play a role in creating a sense of safety and promote accurate understanding of the client’s situation and options. Such issues therefore must be addressed sensitively at the outset and throughout the assessment process.
The consensus panel identified five key concepts that underlie effective engagement during the initial clinical contact: universal access (“no wrong door”), empathic detachment, person-centered assessment, cultural sensitivity, and trauma sensitivity. All staff, as well as substance abuse treatment and mental health clinicians, in any service setting need to develop competency in engaging and welcoming individuals with COD. It is also important to note that while engagement is presented here as the first necessary step for assessment to take place, in a larger sense engagement represents an ongoing concern of the counselor—to understand the client’s experience and to keep him or her positive and engaged relative to the prospect of better health and recovery.
No wrong door
“No wrong door” refers to formal recognition by a service system that individuals with COD may enter a range of community service sites; that they are a high priority for engagement in treatment; and that proactive efforts are necessary to welcome them into treatment and prevent them from falling through the cracks. Substance abuse and mental health counselors are encouraged to identify individuals with COD, welcome them into the service system, and initiate proactive efforts to help them access appropriate treatment in the system, regardless of their initial site of presentation. The recommended attitude is as follows: The purpose of this assessment is not just to determine whether the client fits in my program, but to help the client figure out where he or she fits in the system of care, and to help him or her get there.
Twelve Steps in the Assessment Process
Step 1: Engage the client
Step 2: Identify and contact collaterals (family, friends, other providers) to gather additional information
Step 3: Screen for and detect COD
Step 4: Determine quadrant and locus of responsibility
Step 5: Determine level of care
Step 6: Determine diagnosis
Step 7: Determine disability and functional impairment
Step 8: Identify strengths and supports
Step 9: Identify cultural and linguistic needs and supports
Step 10: Identify problem domains
Step 11: Determine stage of change
Step 12: Plan treatment
Empathic detachment
Empathic detachment requires the assessing clinician to
- Acknowledge that the clinician and client are working together to make decisions to support the client’s best interest
- Recognize that the clinician cannot transform the client into a different person, but can only support change that he or she is already making
- Maintain empathic connection even if the client does not seem to fit into the clinician’s expectations, treatment categories, or preferred methods of working
In the past, the attitude was that the client with COD was the exception. Today, clinicians should be prepared to demonstrate responsiveness to the requirements clients with COD present. Counselors should be careful not to label mental health symptoms immediately as caused by addiction, but instead should be comfortable with the strong possibility that a mental-health condition may be present independently and encourage disclosure of information that will help clarify the meaning of any COD for that client.
Person-centered assessment
Person-centered assessment emphasizes that the focus of initial contact is not on filling out a form or answering several questions or on establishing program fit, but rather on finding out what the client wants, in terms of his or her perception of the problem, what he or she wants to change, and how he or she thinks that change will occur. Mee-Lee (1998) has developed a useful guide that illustrates the types of questions that might be asked in a person-centered assessment in an addiction setting (see Figure 4-1, p. 74). (It should be noted, however, that this is not a validated tool.) While each step in this decision tree leads to the next, the final step can lead back to a previous step, depending on the client’s progress in treatment.
Answers to some of these important questions inevitably will change over time. As the answers change, adjustments in treatment strategies may be appropriate to help the client continue to engage in the treatment process.
Sensitivity to culture, gender, and sexual orientation
An important component of a person-centered assessment is the continual recognition that culture plays a significant role in determining the client’s view of the problem and the treatment. (For a comprehensive discussion of culturally sensitive assessment strategies in addiction settings, see the forthcoming TIP Improving Cultural Competence in Substance Abuse Treatment [CSAT in development a]). With regard to COD, clinicians must remember that ethnic cultures may differ significantly in their approach to substance use disorders and mental disorders, and that this may affect how the client presents. In addition, clients may participate in treatment cultures (12-Step recovery, Dual Recovery Self-Help, psychiatric rehabilitation) that also may affect how they view treatment. Cultural sensitivity also requires recognition of one’s own cultural perspective and a genuine spirit of inquiry into how cultural factors influence the client’s request for help. (See also chapter 2 for a discussion of culturally competent treatment.)
During the assessment process, it is important to ascertain the individual’s sexual orientation as part of the counselor’s appreciation for the client’s personal identity, living situation, and relationships. Counselors also should be aware that women often have family-related and other concerns that must be addressed to engage them in treatment, such as the need for child care. See chapter 7 of this TIP for a more extended consideration of women with COD as a population with specific needs. More information about women’s issues is provided in the forthcoming TIP Substance Abuse Treatment: Addressing the Specific Needs of Women (CSAT in development b).
Trauma sensitivity
The high prevalence of trauma in individuals with COD requires that the clinician consider the possibility of a trauma history even before the assessment begins. Trauma may include early childhood physical, sexual, or emotional abuse; experiences of rape or interpersonal violence as an adult; and traumatic experiences associated with political oppression, as might be the case in refugee or other immigrant populations. This pre-interview consideration means that the approach to the client must be sensitive to the possibility that the client has suffered previous traumatic experiences that may interfere with his or her ability to be trusting of the counselor. Clinicians who observe guardedness on the part of the client should consider the possibility of trauma and try to promote safety in the interview through providing support and gentleness, rather than trying to “break through” evasiveness that erroneously might look like resistance or denial. All questioning should avoid “retraumatizing” the client—see section on trauma screening later in this chapter and, for additional details, see the forthcoming TIP Substance Abuse Treatment and Trauma (CSAT in development d).
Figure 4-1
Assessment Considerations
Engagement:
- What does the client want?
- What is the treatment contract?
- What are the immediate needs?
- What are the multiaxial DSM-IV diagnoses?
Multidimensional severity/level of functioning profile:
- Identify which assessment dimensions are most severe to determine treatment priorities.
- Choose a specific priority for each medium/severe dimension.
What specific services are needed to address these priorities?
What “dose” or intensity of services is needed?
Where can these services be provided in the least intensive, but safe, level of care or site of care?
How will outcomes be measured?
What is the progress of the treatment plan and placement decision?
Source: Adapted from Mee-Lee 1998.
Assessment Step 2: Identify and Contact Collaterals (Family, Friends, Other Providers) To Gather Additional Information
Clients presenting for substance abuse treatment, particularly those who have current or past mental health symptoms, may be unable or unwilling to report past or present circumstances accurately. For this reason, it is recommended that all assessments include routine procedures for identifying and contacting any family and other collaterals who may have useful information to provide. Information from collaterals is valuable as a supplement to the client’s own report in all of the assessment steps listed in the remainder of this chapter. It is valuable particularly in evaluating the nature and severity of mental health symptoms when the client may be so impaired that he or she is unable to provide that information accurately. Note, however, that the process of seeking such information must be carried out strictly in accordance with applicable guidelines and laws regarding confidentiality[1] and with the client’s permission.
Assessment Step 3: Screen for and Detect Co-Occurring Disorders
Because of the high prevalence of co-occurring mental disorders in substance abuse treatment settings, and because treatment outcomes for individuals with multiple problems improve if each problem is addressed specifically, the consensus panel recommends that
- All individuals presenting for substance abuse treatment should be screened routinely for co-occurring mental disorders.
- All individuals presenting for treatment for a mental disorder should be screened routinely for any substance use disorder.
The content of the screening will vary upon the setting. Substance abuse screening in mental health settings should
- Screen for acute safety risk related to serious intoxication or withdrawal
- Screen for past and present substance use, substance related problems, and substance-related disorders
Mental health screening has four major components in substance abuse treatment settings:
- Screen for acute safety risk: suicide, violence, inability to care for oneself, HIV and hepatitis C virus risky behaviors, and danger of physical or sexual victimization
- Screen for past and present mental health symptoms and disorders
- Screen for cognitive and learning deficits
- Regardless of the setting, all clients should be screened for past and present victimization and trauma.
Safety screening
Safety screening requires that early in the interview the clinician specifically ask the client if he or she has any immediate impulse to engage in violent or self-injurious behavior, or if the client is in any immediate danger from others. These questions should be asked directly of the client and of anyone else who is providing information. If the answer is yes, the clinician should obtain more detailed information about the nature and severity of the danger, the client’s ability to avoid the danger, the immediacy of the danger, what the client needs to do to be safe and feel safe, and any other information relevant to safety. Additional information can be gathered depending on the counselor/staff training for crisis/emergency situations and the interventions appropriate to the treatment provider’s particular setting and circumstances. Once this information is gathered, if it appears that the client is at some immediate risk, the clinician should arrange for a more in-depth risk assessment by a mental-health–trained clinician, and the client should not be left alone or unsupervised.
A variety of tools are available for use in safety screening:
- ASAM PPC-2R identifies considerations for immediate risk assessment and recommends follow up procedures (ASAM 2001).
- ASI (McLellan et al. 1992) and Global Appraisal of Individual Needs (GAIN) (Dennis 1998) also include some safety screening questions.
- Some systems use LOCUS (American Association of Community Psychiatrists [AACP] 2000a) as the tool to determine level of care for both mental disorders and addiction. One dimension of LOCUS specifically provides guides for scoring severity of risk of harm. See Potential Risk of Harm on page 77.
None of these tools is definitive for safety screening. Clinicians and programs should use one of these tools only as a starting point, and then elaborate more detailed questions to get all relevant information.
Clinicians should not underestimate risk because the client is using substances actively. For example, although people who are intoxicated might only seem to be making threats of self-harm (e.g., “I’m just going to go home and blow my head off if nobody around here can help me”), all statements about harming oneself or others must be taken seriously. Individuals who have suicidal or aggressive impulses when intoxicated may act on those impulses; remember, alcohol and drug abuse are among the highest predictors of dangerousness to self or others—even without any co-occurring mental disorder. Determining which intoxicated suicidal client is “serious” and which one is not requires a skilled mental health assessment, plus information from collaterals who know the client best. (See chapter 8 and appendix D of this TIP for a more detailed discussion of suicidality.) In addition, it is important to remember that the vast majority of people who are abusing or dependent on substances will experience at least transient symptoms of depression, anxiety, and other mental symptoms. Moreover, it may not be possible, even with a skilled clinician, to determine whether an intoxicated suicidal patient is making a serious threat of self harm; however, safety is a critical and paramount concern. A more detailed discussion of each symptom subgroup is provided in appendix D. Safety screening conducted in mental health settings is highlighted in the text box below.
Screening for past and present mental disorders
Screening for past and present mental disorders has three goals:
- To understand a client’s history and, if the history is positive for a mental disorder, to alert the counselor and treatment team to the types of symptoms that might reappear so that the counselor, client, and staff can be vigilant about the emergence of any such symptoms.
- To identify clients who might have a current mental disorder and need both an assessment to determine the nature of the disorder and an evaluation to plan for its treatment.
- For clients with a current COD, to determine the nature of the symptoms that might wax and wane to help the client monitor the symptoms, especially how the symptoms improve or worsen in response to medications, “slips” (i.e., substance use), and treatment interventions. For example, clients often need help seeing that the treatment goal of avoiding isolation improves their mood—that when they call their sponsor and go to a meeting they break the vicious cycle of depressed mood, seclusion, dwelling on oneself and one’s mood, increased depression, greater isolation, and so on.
Safety Screening in Mental Health Settings
Evaluating safety considerations in mental health settings involves direct questioning of client and collaterals regarding current substance use and/or recent discontinuation of heavy use, along with past and present experiences of withdrawal. If clients obviously are intoxicated, they need to be treated with empathy and firmness, and provision needs to be made for their physical safety. If clients report that they are experiencing withdrawal, or appear to be exhibiting signs of withdrawal, use of formal withdrawal scales can help even inexperienced clinicians to gather information from which medically trained personnel can determine whether medical intervention is required. Such tools include the Clinical Institute Withdrawal Assessment (CIWA-Ar) (Sullivan et al. 1989) for alcohol withdrawal and the Clinical Institute Narcotic Assessment (CINA) (Zilm and Sellers 1978) for opioid withdrawal.
Mental health clinicians need to be aware that not all drugs have a physiological withdrawal associated with them, and it should not be assumed that withdrawal from any drug of abuse will require medical intervention. Only in the case of alcohol, opioids, sedative-hypnotics, or benzodiazepines is medical intervention likely to be required due to the pharmacological properties of the substance.
Potential Risk of Harm
- Risk of Harm: This dimension of the assessment considers a person’s potential to cause significant harm to self or others. While this may most frequently be due to suicidal or homicidal thoughts or intentions, in many cases unintentional harm may result from misinterpretations of reality, from inability to care adequately for oneself, or from altered states of consciousness due to use of intoxicating substances. For the purpose of evaluation in this parameter, deficits in ability to care for oneself are considered only in the context of their potential to cause harm. Likewise, only behaviors associated with substance use are used to rate risk of harm, not the substance use itself. In addition to direct evidence of potentially dangerous behavior from interview and observation, other factors may be considered in determining the likelihood of such behavior such as past history of dangerous behaviors, ability to contract for safety, and availability of means. When considering historical information, recent patterns of behavior should take precedence over patterns reported from the remote past. Risk of harm may be rated according to the following criteria:
Minimal risk of harm:
- No indication of suicidal or homicidal thoughts or impulses, no history of suicidal or homicidal ideation, and no indication of significant distress.
- Clear ability to care for self now and in the past.
Low risk of harm:
- No current suicidal or homicidal ideation, plan, intentions or serious distress, but may have had transient or passive thoughts recently or in the past.
- Substance use without significant episodes of potentially harmful behaviors.
- Periods in the past of self-neglect without current evidence of such behavior.
Moderate risk of harm:
- Significant current suicidal or homicidal ideation without intent or conscious plan and without past history.
- No active suicidal/homicidal ideation, but extreme distress and/or a history of suicidal/homicidal behavior exists.
- History of chronic impulsive suicidal/homicidal behavior or threats and current expressions do not represent significant change from baseline.
- Binge or excessive use of substances resulting in potentially harmful behaviors without current involvement in such behavior.
- Some evidence of self neglect and/or compromise in ability to care for oneself in current environment.
Serious risk of harm:
- Current suicidal or homicidal ideation with expressed intentions and/or past history of carrying out such behavior but without means for carrying out the behavior, or with some expressed inability or aversion to doing so, or with ability to contract for safety.
- History of chronic impulsive suicidal/homicidal behavior or threats with current expressions or behavior representing a significant elevation from baseline.
- Recent pattern of excessive substance use resulting in disinhibition and clearly harmful behaviors with no demonstrated ability to abstain from use.
- Clear compromise of ability to care adequately for oneself or to be aware adequately of environment.
Extreme risk of harm:
- Current suicidal or homicidal behavior or such intentions with a plan and available means to carry out this behavior without expressed ambivalence or significant barriers to doing so; or with a history of serious past attempts which are not of a chronic, impulsive, or consistent nature; or in presence of command hallucinations or delusions which threaten to override usual impulse control.
- Repeated episodes of violence toward self or others, or other behaviors resulting in harm while under the influence of intoxicating substances with pattern of nearly continuous and uncontrolled use.
- Extreme compromise of ability to care for oneself or to monitor adequately the environment with evidence of deterioration in physical condition or injury related to these deficits.
Source: AACP 2000a.
A number of screening, assessment, and treatment planning tools are available to assist the substance abuse treatment team. For assessment of specific disorders and/or for differential diagnosis and treatment planning, there are literally hundreds of assessment and treatment planning tools. NIAAA operates a webbased service that provides quick information about alcoholism treatment assessment instruments and immediate online access to most of them, and the service is updated continually with new information and assessment instruments NIDA has a publication from a decade ago (Rounsaville et al. 1993) that provides broad background information on assessment issues pertinent to COD and specific information about numerous mental health, treatment planning, and substance abuse tools. Of course, NIDA continues to explore issues related to screening and assessment. The mental health field contains a vast array of screening and assessment devices, as well as subfields devoted primarily to the study and development of evaluative methods. Almost all Substance Abuse and Mental Health Services Administration TIPs, which are available online (www.kap.samhsa.gov), have a section on assessment, many have appendices with wholly reproduced assessment tools or information about locating such tools, and TIPs 31, 16, 13, 11, 10, 9, 7, and 6 are centered specifically on assessment issues.
Advanced assessment techniques include assessment instruments for general and specific purposes and advanced guides to differential diagnosis. Most highpower assessment techniques center on a specific type of problem or set of symptoms, such as the BDIII (Beck et al. 1996), the Beck Anxiety Inventory (BAI) (Beck et al. 1988), or the Hamilton Anxiety Scale (Hamilton 1959) or the Hamilton Rating Scale for Depression (Hedlung and Vieweg 1979). There are highpower broad assessment measures such as the Minnesota Multiphasic Personality Inventory2 (MMPI2) (Butcher et al. 2001). However, such assessment devices typically are lengthy (the MMPI is more than 500 items), often require specific doctoral training to use, and can be difficult to adapt properly for some substance abuse treatment settings.
For both clinical and research activities, there are a number of wellknown and widely used guides to the differential diagnostic process in the mental health field, such as the Structured Clinical Interview for Diagnosis (SCID). Again, the SCIDs involve considerable time and training, with a separate SCID for Axis I, Axis II, and dissociative disorders. Other broad highpower diagnostic tools are the Diagnostic Interview Schedule (DIS) and the Psychiatric Research Interview for Substance and Mental Disorders (PRISM), but these methods can require 1 to 3 hours and extensive training. These tools generally provide information beyond the requirements of most substance abuse treatment programs.
When using any of the wide array of tools that detect symptoms of mental disorders, counselors should bear in mind that symptoms of mental disorder can be mimicked by substances. For example, hallucinogens may produce symptoms that resemble psychosis, and depression commonly occurs during withdrawal from many substances. Even with well-tested tools, it can be difficult to distinguish between a mental disorder and a sub-stance-related disorder without additional information such as the history and chronology of symptoms. In addition to interpreting the results of such instruments in the broader context of what is known about the client’s history, counselors also are reminded that retesting often is important, particularly to confirm diagnostic conclusions for clients who have used substances.
The section below briefly highlights some available instruments available for mental health screening.
Mental Health Screening Form-III
The Mental Health Screening Form-III (MHSF-III) has only 18 simple questions and is designed to screen for present or past symptoms of most of the main mental disorders (Carroll and McGinley 2001). It is available to the public at no charge from the Project Return Foundation, Inc. and it is reproduced in its entirety in appendix H, along with instructions for its use and contact information (a Spanish form and instructions can be downloaded). The MHSF-III was developed within a substance abuse treatment setting and it has face validity—that is, if a knowledgeable diagnostician reads each item, it seems clear that a “yes” answer to that item would warrant further evaluation of the client for the mental disorder for which the item represents typical symptomatology.
On the other hand, the MHSF-III is only a screening device as it asks only one question for each disorder for which it attempts to screen. If a client answers “no” because of a misunderstanding of the question or a momentary lapse in memory or test-taking attitude, the screen would produce a “falsenegative,” where the client might have the mental disorder but the screen falsely indicates that the person probably does not have the disorder. In a journal article the MHSFIII is referred to as a “rough screening device” (Carroll and McGinley 2001, p. 35), and the authors make suggestions about its use, comments about its limitations, and review favorable validity and reliability data.
Mini-International Neuropsychiatric Interview
For a more complete screening instrument, the Mini-International Neuropsychiatric Interview (M.I.N.I.) is a simple 15- to 30- minute device that covers 20 mental dis-orders, including substance use disorders. Considerable validation research has accumulated on the M.I.N.I. (Sheehan et al. 1998).
Counselors should bear in mind that symptoms of mental disorder can be mimicked by substances.
For each disorder the M.I.N.I. has an ordered series of about 6 to 12 questions, and it has a simple and immediate scoring procedure. For example, in terms of suicidality the M.I.N.I. contains questions about whether in the past month the client has
- Thought about being better off dead or wishing to be dead (1 point)
- Wanted to harm himself/herself (2 points)
- Thought about suicide (6 points)
- Attempted suicide (10 points)
- Developed a suicide plan (10 points)
M.I.N.I. contains a sixth question asking if the client has ever attempted suicide (4 points). Scoring rates low current suicide risk as 1 to 5 points, moderate as 6 to 9 points, and high as 10 or more points.
The M.I.N.I. family consists of
- The M.I.N.I. (a low-power, broad screening device to see if the client requires further assessment)
- A two-page M.I.N.I. screen for research purposes or when time is limited
- The M.I.N.I. Plus (an expanded version of the M.I.N.I. designed specifically to determine whether symptoms were associated with alcohol and other drug use and/or periods of abstinence)
- The M.I.N.I. Tracking (a 17-page document that provides symptom descriptors that can be used to monitor a client’s progress in treatment, monitor how a client’s symptoms are affected by treatment interventions or medications or other factors, and help with documenting where, when, and why changes occur)
Brief Symptom Inventory-18
Another proprietary instrument that can be used to track clients from session to session or over longer periods of time is the Brief Symptom Inventory-18 (BSI-18). The BSI-18 questionnaire contains 18 items and asks clients to rate each question on a five-point scale. In addition to a Global Severity Index score, there are separate scores for anxiety, depression, and somatization subscales. The BSI-18 was derived from the 53-item Brief Symptom Inventory, which was derived from the Symptom Checklist-90-Revised (SCL-90-R) (Derogatis 1975), and the 15-item SDS (McCorkle and Young 1978) also was a derivative of the BSI that has been superceded by the relatively new BSI-18.
ASI
The ASI (McLellan et al. 1992) does not screen for mental disorders and provides only a low-power screen for generic mental health problems. Use of the ASI ranges widely, with some substance abuse treatment programs using a scaled-down approach to gather basic information about a client’s alcohol use, drug use, legal status, employment, family/social, medical, and psychiatric status, to an in-depth assessment and treatment planning instrument to be administered by a trained interviewer who makes complex judgments about the client’s presentation and ASI-taking attitudes. Counselors can be trained to make clinical judgments about how the client comes across, how genuine and legitimate the client’s way of responding seems, whether there are any safety or self-harm concerns requiring further investigation, and where the client falls on a nine-point scale for each dimension. With about 200 items, the ASI is a low-power instrument but with a very broad range, covering the seven areas mentioned above and requiring about 1 hour for the interview. Development of and research into the ASI continues, including training programs, computerization, and critical analyses. It is a public domain document that has been used widely for 2 decades. It is reproduced in TIP 38 as appendix D (CSAT 2000c, pp. 193–204), and information about obtaining the manual for the ASI and up-to-date information is in appendix G. Over the past several years, NIDA’s Clinical Trials Network (CTN) has been researching both the use of and the training for the ASI.
Screening for past and present substance use disorder
This section is intended primarily for counselors working in mental health service settings. It suggests ways to screen clients for substance abuse problems.
Screening begins with inquiry about past and present substance use and substance-related problems and disorders. If the client answers yes to having problems and/or a disorder, further assessment is warranted. It is important to remember that if the client acknowledges a past substance problem but states that it is now resolved, assessment is still required. Careful exploration of what current strategies the individual is using to prevent relapse is warranted. Such information can help ensure that those strategies continue while the individual is focusing on mental health treatment.
Screening for the presence of substance abuse symptoms and problems involves four components:
- Substance abuse symptom checklists
- Substance abuse severity checklists
- Formal screening tools that work around denial
- Screening of urine, saliva, or hair samples
Symptom checklists: These include checklists of common categories of substances, history of associated problems with use, and a history of meeting criteria for substance dependence for that substance. It is not helpful to develop checklists that are overly detailed, because they begin to lose value as simple screening tools. It is helpful to remember to include abuse of over-the-counter medication (e.g., cold pills), abuse of prescribed medication, and gambling behavior in the checklist. It also is reasonable to screen for compulsive sexual behavior, Internet addiction, and compulsive spending.
Severity checklists: It is useful to monitor the severity of substance use disorder (if present) and to determine the possible presence of dependence. This process can begin with simple questions about past or present diagnosis of substance dependence, and the client’s experience of associated difficulties. Some programs may use formal substance use disorder diagnostic tools; others use the ASI (McLellan et al. 1992) or similar instrument, even in the mental health setting. The New Hampshire Dartmouth Psychiatric Research Center has developed clinician-rated alcohol-and drug-use scales for monitoring substance abuse severity in individuals with mental disorders: the Alcohol Use Scale (AUS) and Drug Use Scale (DUS) (Drake et al. 1996b) and others.
Screening tools: Most common substance abuse screening tools have been used with individuals with COD. These include the
CAGE (Mayfield et al. 1974), the Michigan Alcoholism Screen Test (MAST) (Selzer 1971), the Drug Abuse Screening Test (DAST) (Skinner 1982), and the Alcohol Use Disorders Identification Test (AUDIT) (Babor et al. 1992). The Dartmouth Assessment of Lifestyle Inventory (DALI) is used routinely as a screening tool in some research settings working with individuals with serious mental disorders (Rosenberg et al. 1998).
The SSI-SA was developed by the consensus panel of TIP 11, Simple Screening Instruments for Outreach for Alcohol and Other Drug Abuse and Infectious Diseases (CSAT 1994c). The SSI-SA is reproduced in its entirety in appendix H. It is a 16-item scale, although only 14 items are scored so that scores can range from 0 to 14. These 14 items were selected by the TIP 11 consensus pan-elists from existing alcohol and drug abuse screening tools. A score of 4 or greater has become the established cut-off point for warranting a referral for a full assessment. Since its publication in 1994 the SSI-SA has been widely used and its reliability and validity investigated. For example, Peters and colleagues (2004) reported on a national survey of correctional treatment for COD. Reviewing 20 COD treatment programs in correctional settings from 13 States, the SSISA was identified as among the most common screening instruments used. For more information, see appendix H.
Screening begins with inquiry about past and present substance use and substance-related problems and disorders.
Toxicology screening: Given the high prevalence of substance use disorders in patients with mental health problems, the routine use of urine or other screening is indicated for all new mental health clients. It especially is suggested in settings in which the likelihood of clients regularly presenting unreliable information is particularly great; for example, in adolescent and/or criminal justice settings. Use of urine screening is highly recommended whenever the clinical presentation does not seem to fit the client’s story, or where there appear to be unusual mental status symptoms or changes not explained adequately. Saliva testing may be less intrusive than hair or urine testing in patients who are shy or who are extremely paranoid.
Trauma screening
Research projects focusing on the needs of people with COD who are victims of trauma have led to the development of specific screening tools to identify trauma in treatment populations. To screen for posttraumatic stress disorder (PTSD), assuming the client has a trauma, the Modified PTSD Symptom Scale: Self-Report Version would be a good choice (this instrument can be found in TIP 36, Substance Abuse Treatment for Persons With Child Abuse and Neglect Issues [CSAT 2000d, p. 170]). This scale also is useful for monitoring and tracking PTSD symptoms over time. The PTSD Checklist (Blanchard et al. 1996) is a validated instrument that substance abuse treatment agencies also may find useful in trauma screening.
It is important to emphasize that in screening for a history of trauma or in obtaining a preliminary diagnosis of PTSD, it can be damaging to ask the client to describe traumatic events in detail. To screen, it is important to limit questioning to very brief and general questions, such as “Have you ever experienced childhood physical abuse? Sexual abuse? A serious accident? Violence or the threat of it? Have there been experiences in your life that were so traumatic they left you unable to cope with day-to-day life?” See the discussion of screening and assessment for PTSD in appendix D for more complete information.
Assessment Step 4: Determine Quadrant and Locus of Responsibility
Determination of quadrant assignment is based on the severity of the mental and substance use disorders (see chapter 2 for a detailed discussion of the four-quadrant model). Most of the information needed for this determination will have been acquired during step 2, but there are a few added nuances. Quadrant determination may be specified formally by procedures in certain States. For example, New York has drafted (but not yet adopted) a set of objective criteria for determining at screening who should be considered as belonging in quadrant IV. Where no such formal procedures are present, the following sequence may be useful and is certainly within the capability of substance abuse treatment clinicians in any setting.
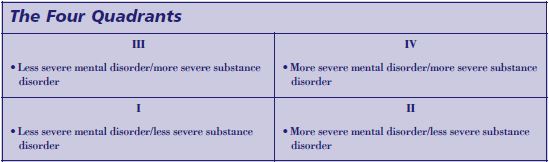
Assessment Step 4—Application to Case Examples
Cases 1 and 2. Both Maria M. and George T. are examples of clients with serious addiction who also have serious mental disorders, but do not appear to be seriously disabled. They would therefore meet criteria for quadrant III and should be placed in programs for people who have less serious mental disorders and more serious substance use disorders. Note that though the diagnosis of bipolar disorder is typically considered a serious mental illness, the quadrant system emphasizes the acute level of disability/severity of the mental and substance use disorders of the individual, rather than relying solely on diagnostic classification.
Case 3. Jane B., the homeless woman with paranoid schizophrenia, generally would meet criteria for serious and persistent mental illness in almost every State, based on the severity of the diagnosis and disability, combined with the persistence of the disorder. Jane B. also has serious addiction. In the quadrant model, if she already has been identified as a mental health priority client (e.g., has a mental health case manager), she would be considered quadrant IV, and referral for mental health case management services would be important.
Determination of serious mental illness (SMI) status
Every State mental health system has developed a set of specific criteria for determining who can be considered seriously mentally ill (and therefore eligible to be considered a mental health priority client). These criteria are based on combinations of specific diagnoses, severity of disability, and duration of disability (usually 6 months to 1 year). Some require that the condition be independent of a substance use disorder. These criteria are different for every State. It would be helpful for substance abuse treatment providers to obtain copies of the criteria for their own States, as well as copies of the specific procedures by which eligibility is established by their States’ mental health systems. By determining that a client might be eligible for consideration as a mental health priority client, the substance abuse treatment counselor can assist the client in accessing a range of services and/or benefits that the client may not know is open to her or him.
Determining SMI status begins with finding out if the client already is receiving mental health priority services (e.g., Do you have a mental health case manager? Are you a Department of Mental Health client?).
- If the client already is a mental health client, then he or she will be assigned to quadrant II or IV. Contact needs to be made with the mental health case manager and a means of collaboration established to promote case management.
- If the client is not already a mental health client, but appears to be eligible and the client and family are willing, referral for eligibility determination should be arranged.
- Clients who present in addiction treatment settings who look as if they might be SMI, but have not been so determined, should be considered to belong to quadrant IV.
For assistance in determination of the severity of symptoms and disability, the substance abuse treatment clinician can use the Dimension 3 (Emotional/Behavioral) subscales in the ASAM PPC-2R or LOCUS, especially the levels of severity of comorbidity and impairment/functionality.
Determination of severity of substance use disorders
Presence of active or unstable substance dependence or serious substance abuse (e.g., recurrent substance-induced psychosis without meeting other criteria for dependence) would identify the individual as being in quadrant III or IV. Less serious substance use disorder (mild to moderate substance abuse; substance dependence in full or partial remission) identifies the individual as being in quadrant I or II.
If the client is determined to have SMI with serious substance use disorder, he falls in quadrant IV; those with SMI and mild substance use disorder fall in quadrant II. A client with serious substance use disorder who has mental health symptoms that do not constitute SMI falls into quadrant III. A client with mild to moderate mental health symptoms and less serious substance use disorder falls into quadrant I.
Clients in quadrant III who present in substance abuse treatment settings are often best managed by receiving care in the addiction treatment setting, with collaborative or consultative support from mental health providers. Individuals in quadrant IV usually require intensive intervention to stabilize and determination of eligibility for mental health services and appropriate locus of continuing care. If they do not meet criteria for SMI, once their more serious mental symptoms have stabilized and substance use is controlled initially, they begin to look like individuals in quadrant III, and can respond to similar services.
Note, however, that this discussion of quadrant determination is not validated by clinical research. It is merely a practical approach to adapting an existing framework for clinical use, in advance of more formal processes being developed, tested, and disseminated.
In many systems, the process of assessment stops largely after assessment step 4 with the determination of placement. Some information from subsequent steps (especially step 7) may be included in this initial process, but usually more in-depth or detailed consideration of treatment needs may not occur until after “placement” in an actual treatment setting.
Assessment Step 5: Determine Level of Care
The use of the ASAM PPC-2R provides a mechanism for an organized assessment of individuals presenting for substance use disorder treatment to determine appropriate placement in “level of care.” This process involves consideration of six dimensions of assessment:
- Dimension 1: Acute Intoxication and/or Withdrawal Potential
- Dimension 2: Biomedical Conditions and Complications
- Dimension 3: Emotional, Behavioral, or Cognitive Conditions and Complications
- Dimension 4: Readiness to Change
- Dimension 5: Relapse, Continued Use, or Continued Problem Potential
- Dimension 6: Recovery/Living Environment
The ASAM PPC2R (ASAM 2001) evaluates level of care requirements for individuals with COD. Dimension 3 encompasses “Emotional, Behavioral or Cognitive Conditions and Complications.” Five areas of risk must be considered related to this dimension (ASAM 2001, pp. 283–284):
- Suicide potential and level of lethality
- Interference with addiction recovery efforts (“The degree to which a patient is distracted from addiction recovery efforts by emotional, behavioral and/or cognitive problems and conversely, the degree to which a patient is able to focus on addiction recovery”)
- Social functioning
- Ability for selfcare
- Course of illness (a prediction of the patient’s likely response to treatment)
Consideration of these dimensions permits the client to be placed in a particular level on a continuum of services ranging from intensive case management for individuals with serious mental disorders who are not motivated to change (Level I.5) to psychiatric inpatient care (Level IV). In addition, there is the capacity to distinguish, at each level of care, individuals with lower severity of mental symptoms or impairments that require standard or Dual Diagnosis Capable programming at that level of care from individuals with moderately severe symptoms or impairments that require Dual Diagnosis Enhanced programming at that level of care. (See below for assessment of the level of impairment.) The ASAM PPC have undergone limited validity testing in previous versions, are used to guide addiction treatment matching in more than half the States, and are influential in almost all of the rest.
Tools: The LOCI–2R (Hoffmann et al. 2001) is a proprietary tool designed specifically to perform a structured assessment for level of care placement based on ASAM PPC2R levels of care (ASAM 2001). The GAIN (Dennis 1998) is another broad set of tools and training developed within an addiction setting; however, GAIN products are also proprietary.
In some systems, the LOCUS Adult Version 2000 (AACP 2000a) is being introduced as a systemwide level of care assessment instrument for either mental health settings only, or for both mental health and substance abuse treatment settings. Like the ASAM, LOCUS uses multiple dimensions of assessment:
- Risk of Harm
- Functionality
- Comorbidity (Medical, Addictive, Psychiatric)
- Recovery Support and Stress
- Treatment Attitude and Engagement
- Treatment History
LOCUS is simpler to use than ASAM PPC2R. It has a point system for each dimension that permits aggregate scoring to suggest level of service intensity. LOCUS also permits level of care assessment for individuals with mental disorders or substance use disorders only, as well as for those with COD. Some pilot studies of LOCUS have supported its validity and reliability. However, compared to ASAM PC2R, LOCUS is much less sensitive to the needs of individuals with substance use disorders and has greater difficulty distinguishing the separate contributions of mental and substancerelated symptoms to the clinical picture.
Assessment Step 5—Application to Case Examples
Case 3. The severity of Jane B.’s condition and her psychosis, homelessness, and lack of stability may lead the clinician initially to consider psychiatric hospitalization or referral for residential substance abuse treatment. In fact, application of assessment criteria in ASAM PPC-2R might have led easily to that conclusion. In ASAM PPC-2R, more flexible matching is possible. The first consideration is whether the client meets criteria for involuntary psychiatric commitment (usually, suicidal or homicidal impulses, or inability to feed oneself or obtain shelter). In this instance, she is psychotic and homeless but has been able to find food and shelter; she is unwilling to accept voluntary mental health services. Further, residential substance abuse treatment is inappropriate, both because she is completely unmotivated to get help and because she is likely to be too psychotic to participate in treatment effectively. ASAM PPC-2R would therefore recommend Level I.5 intensive mental disorder case management as described above.
If after extended participation in the engagement strategies described earlier, she began to take antipsychotic medication, after a period of time her psychosis might clear up, and she might begin to express interest in getting sober. In that case, if she had determined that she is unable to get sober on the street, residential substance abuse treatment would be indicated. Because of the longstanding severity of her mental illness, it is likely that she would continue to have some level of symptoms of her mental disorder and disability even when medicated. In this case, Jane B. probably would require a residential program able to supply an enhanced level of services.
Assessment Step 6: Determine Diagnosis
Determining the diagnosis can be a formidable clinical challenge in the assessment of COD. Clinicians in both mental health services and substance abuse treatment settings recognize that it can be impossible to establish a firm diagnosis when confronted with the mixed presentation of mental symptoms and ongoing substance abuse. Of course, substance abuse contributes to the emergence or severity of mental symptoms and therefore confounds the diagnostic picture. Therefore, this step often includes dealing with confusing diagnostic presentations.
Addiction counselors who want to improve their competencies to address COD are urged to become conversant with the basic resource used to diagnose mental disorders, the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSMIV-TR) (American Psychiatric Association 2000).
The importance of client history
- Principle #1: Diagnosis is established more by history than by current symptom presentation. This applies to both mental and substance use disorders.
The first step in determining the diagnosis is to determine whether the client has an established diagnosis and/or is receiving ongoing treatment for an established disorder. This information can be obtained by the counselor as part of the routine intake process. If there is evidence of a disorder but the diagnosis and/or treatment recommendations are unclear, the counselor immediately should begin the process of obtaining this information from collaterals. If there is a valid history of a mental disorder diagnosis at admission to substance abuse treatment, that diagnosis should be considered presumptively valid for initial treatment planning, and any existing stabilizing treatment should be maintained. In addition to confirming an established diagnosis, the client’s history can provide insight into patterns that may emerge and add depth to knowledge of the client.
For example, if a client comes into the clinician’s office under the influence of alcohol, it is reasonable to suspect alcohol dependence, but the only diagnosis that can be made based on that datum is “alcohol intoxication.” It is important to note that this warrants further investigation; on the one hand, false positives can occur, while on the other, detoxification may be needed. Conversely, if a client comes into the clinician’s office and has not had a drink in 10 years, attends Alcoholics Anonymous (AA) meetings three times per week, and had four previous detoxification admissions, the clinician can make a diagnosis of alcohol dependence (in remission at present). Moreover, the clinician can predict that 20 years from now that client will still have the diagnosis of alcohol dependence since the history of alcohol dependence and treatment sustains a lifetime diagnosis of alcohol dependence.
Assessment Step 6—Application to Case Examples
Case 2. George T. has cocaine dependence and bipolar disorder stabilized with lithium. He reports that when he uses cocaine he has mood swings, but that these go away when he stops using for a while, as long as he takes his medication. At the initial visit, George T. states he has not used for a week and has been taking his medication regularly. He displays no significant symptoms of mania or depression and appears reasonably calm. The counselor should not conclude that because George T. has no current symptoms the diagnosis of bipolar disorder is incorrect, or that all the mood swings are due to cocaine dependence. At initial contact, the presumption should be that the diagnosis of bipolar disorder is accurate, and lithium needs to be maintained.
Case 1. Maria M., the 38-year-old Hispanic/Latina female with cocaine and opioid dependence, initially was receiving methadone maintenance treatment only. She also used antidepressants prescribed by her outside primary care physician. She presented to methadone maintenance program staff with complaints of depression. Maria M. reported that since treatment with methadone (1 year) she had not used illicit opioids. However, she stated that when she does not use cocaine, she often feels depressed “for no reason.” Nevertheless, she has many stressors involving her children, who also have drug problems. She reports that depression is associated with impulses to use cocaine, and consequently she has recurrent cocaine binges. These last a few days and are followed by persistent depression.
What is the mental diagnosis? To answer this question it is important to obtain a mental disorder history that relates mental symptoms to particular time periods and patterns of substance use and abuse.
The client’s history reveals that although she grew up with an abusive father with an alcohol problem, she herself was not abused physically or sexually. Although hampered by poor reading ability, she stayed in school with no substance abuse until she became pregnant at age 16 and dropped out of high school. Despite becoming a single mother at such a young age, she worked three jobs and functioned well, while her mother helped raise the baby. At age 23, she began a 9-year relationship with an abusive person with an alcohol and illicit drug problem, during which time she was exposed to a period of severe trauma and abuse. She is able to recall that during this relationship, she began to lose her self-esteem and experience persistent depression and anxiety.
She began using cocaine at age 27, initially to relieve those symptoms. Later, she lost control and became addicted. Four years ago, she was first diagnosed as having major depression, and was prescribed antidepressant medication, which she found helpful. Two years ago, she began using opioids, became addicted, and then entered methadone treatment. She receives no specific treatment for cocaine dependence. She has noticed that her depression persists during periods of cocaine and opioid abstinence lasting more than 30 days. On one occasion, during one of these periods, her medication ran out, and she noticed her depression became much worse. Even at her baseline, she remains troubled by lack of self-confidence and fearfulness, as well as depressed mood.
Her depression persists during periods of more than 30 days of abstinence and responds to some degree to antidepressants. The fact that her depression persists even when she is abstinent and responds to antidepressants suggests strongly a co-occurring affective disorder. There are also indications of the persistent effects of trauma, possibly posttraumatic stress disorder. Trauma issues have never been addressed. Her opioid dependence has been stabilized with methadone. She has resisted recommendations to obtain more specific treatment for cocaine dependence.
Similarly, if a client comes into the clinician’s office and says she hears voices (whether or not the client is sober currently), no diagnosis should be made on that basis alone. There are many reasons people hear voices. They may be related to substance-related syndromes (e.g., substance-induced psychosis or hallucinosis, which is the experience of hearing voices that the client knows are not real, and that may say things that are distressing or attacking—particularly when there is a trauma history—but are not bizarre). With COD, most causes will be independent of substance use (e.g., schizophrenia, schizoaffective disorder, affective disorder with psychosis or dissociative hallucinosis related to PTSD). Psychosis usually involves loss of ability to tell that the voices are not real, and increased likelihood that they are bizarre in content. Methamphetamine psychosis is particularly confounding because it can mimic schizophrenia. Many individuals with psychotic disorders will still hear voices when on medication, but the medication makes the voices less bizarre and helps the client know they are not real.
If the client states he has heard voices, though not as much as he used to, that he has been clean and sober for 4 years, that he remembers to take his medication most days though every now and then he forgets, and that he had multiple psychiatric hospitalizations for psychosis 10 years ago but none since, then the client clearly has a diagnosis of psychotic illness (probably schizophrenia or schizoaffective disorder). Given the client’s continuing symptoms while clean and sober and on medication, it is quite possible that the diagnosis will persist.
Documenting prior diagnoses
- Principle #2: It is important to document prior diagnoses and gather information related to current diagnoses, even though substance abuse treatment counselors may not be licensed to make a mental disorder diagnosis.
Diagnoses established by history should not be changed at the point of initial assessment. If the clinician has a suspicion that a long-established diagnosis may be invalid, it is important that he or she takes time to gather additional information, consult with collaterals, get more careful and detailed history (see below), and develop a better relationship with the client before recommending diagnostic re-evaluation. It is important for the counselor to raise issues related to diagnosis with the clinical supervisor or at a team meeting.
In many instances, of course, no well-established mental disorder diagnosis exists, or multiple diagnoses give a confusing picture. Even when there is an established diagnosis, it is helpful to gather information to confirm that diagnosis. During the initial assessment process, substance abuse treatment counselors can gather data that can assist in the diagnostic process, either by supporting the findings of the existing mental health assessment, or providing useful background information in the event a new mental health assessment is conducted. The key to doing this is not merely to gather lists of past and present symptoms, but to connect those symptoms to key time periods in the client’s life that are helpful in the diagnostic process— namely, before the onset of a substance use disorder and during periods of abstinence (or during periods of very limited use) or those that occur after the onset of the substance use disorder and persist for more than 30 days.
The clinician also must seek to determine whether mental symptoms occur only when the client is using substances actively. Therefore, it is important to determine the nature and severity of the symptoms of the mental disorder when the substance disorder is stabilized.
Linking mental symptoms to specific periods
- Principle #3: For diagnostic purposes, it is almost always necessary to tie mental symptoms to specific periods of time in the client’s history, in particular those times when active substance use disorder was not present.
Unfortunately, most substance abuse assessment tools are not structured to require connection of mental symptoms to such periods of use or abstinence. For this reason, mental disorder symptom information obtained from such tools can be confusing and often contributes to counselors feeling the whole process is not worth the effort. In fact, it is striking that when clinicians seek information about mental symptoms during periods of abstinence, such information is almost never part of traditional assessment forms. The mental history and substance use history have in the past been collected separately and independently. As a result, the opportunity to evaluate interaction, which is the most important diagnostic information beyond the history, has been routinely lost. Newer and more detailed assessment tools overcome these historical, unnecessary divisions.
One instrument that may be helpful in this regard is the M.I.N.I. Plus (described above), which has a structure to connect any identified symptoms to periods of abstinence. Clinicians can use this information to distinguish substance-induced mental disorders from independent mental disorders. Drake and others in their work on mental disorder treatment teams in New Hampshire have adapted the Timeline Follow Back Method, developed by Sobell and Mueser (Mueser et al. 1995b; Sobell et al. 1979), that can be used with individuals who have serious mental disorders and substance use disorders. More detailed mental health research diagnostic tools (e.g., the SCID) encourage a similar process.
Consequently, the substance abuse treatment counselor can proceed in two ways:
- Inquire whether any mental symptoms or treatments identified in the screening process were present during periods of 30 days of abstinence or longer, or were present before onset of substance use. (“Did this symptom or episode occur during a period when you were clean and sober for at least 30 days?”)
- Define with the client specific time periods where substance use disorder was in remission, and then get detailed information about mental symptoms, diagnoses, impairments, and treatments during those periods of time. (“Can you recall a specific period when you were not using? Did these symptoms [or whatever the client has reported]
occur during that period?”) This approach may yield more reliable information.
During this latter process, the counselor can use one of the medium-power symptom screening tools as a guide. Alternatively, the counselor can use the handy outlines of the DSM-IV criteria for common disorders and inquire whether those criteria symptoms were met, whether they were diagnosed and treated, and if so, with what methods and how successfully. This information can suggest or support the accuracy of diagnoses. Documentation also can facilitate later diagnostic assessment by a mental-health–trained clinician.
Assessment Step 7: Determine Disability and Functional Impairment
Determination of both current and baseline functional impairment contributes to identification of the need for case management and/or higher levels of support. This step also relates to the determination of level of care requirements. Assessment of current cognitive capacity, social skills, and other functional abilities also is necessary to determine if there are deficits that may require modification in the treatment protocols of relapse prevention efforts or recovery programs. For example, the counselor might inquire about past participation in special education or related testing.
Assessment Step 7—Application to Case Example
Case 1. Assessment of Maria M.’s functional capacity at baseline indicated that she could read only at a second grade level. Consequently, educational materials presented in written form needed to be presented in alternative formats. These included audiotapes and videos to teach her about addiction, depression, trauma, and recovery from these conditions. In addition, Maria M.’s history of trauma (previously discussed) led her to experience anxiety in large group situations, particularly where men were present. This led her counselor to recommend attending 12-Step meetings that were smaller and/or women only. The counselor also suggested that she attend in the company of female peers. Further, the clinician referred her to trauma-specific counseling.
Case 3. Once Jane B. had begun to stabilize on medication and expressed interest in residential addiction treatment, it became necessary to assess her ability to participate in standard dual diagnosis capable (DDC) treatment versus her need for more dual diagnosis enhanced (DDE) treatment. Jane B. was still living in a shelter, but was able to maintain her personal hygiene and dress appropriately now that she was on medication. She looked somewhat suspicious and guarded, but could answer questions appropriately and denied having hallucinations.
To determine her ability to succeed in standard residential substance abuse treatment, her counselor asked her to attend an AA meeting. The clinician also asked her to complete an assignment to read some substance abuse literature and write down what she had learned. The client reported that she was nervous at the meeting but was able to stay the whole time. She said that she related well to what one of the speakers was saying. She also completed the written assignment quite well; it turned out she was very bright and had completed 1 year of college. Noting that she was complying with medication and her mental status was stable, the counselor felt comfortable referring her to the DDC program.
Had this client been unable to attend AA without individual support, or if she experienced obvious difficulty with the assignment, it would have been clearer that a program with an enhanced capacity to treat persons with COD would be indicated. If such a program were not available, she would have needed to continue to build skills slowly to address her substance use with the assistance of her outpatient case management program.
Assessing functional capability
Current level of impairment is determined by assessing functional capabilities and deficits in each of the areas listed below. Similarly, baseline level of impairment is determined by identifying periods of extended abstinence and mental health stability (greater than 30 days) according to the methods described in the previous assessment step. The clinician determines:
- Is the client capable of living independently (in terms of independent living skills, not in terms of maintaining abstinence)? If not, what types of support are needed?
- Is the client capable of supporting himself financially? If so, through what means? If not, is the client disabled, or dependent on others for financial support?
- Can the client engage in reasonable social relationships? Are there good social supports? If not, what interferes with this ability, and what supports would the client need?
- What is the client’s level of intelligence? Is there a developmental or learning disability? Are there cognitive or memory impairments that impede learning? Is the client limited in ability to read, write, or understand? Are there difficulties with focusing, concentrating, and completing tasks?
The ASI (McLellan et al. 1992) and the GAIN (Dennis 1998) provide some information about level of functioning for individuals with substance use disorders. They are valuable when supplemented by interview information in the above areas. (Note that the ASI also exists in an expanded version specifically for women [ASI-F, CSAT 1997c].) The counselor also should inquire about any current or past difficulties the client has had in learning or using relapse prevention skills, participating in self-help recovery programs, or obtaining medication or following medication regimens. In the same vein, the clinician may inquire about use of transportation, budgeting, self-care, and other related skills, and their effect on life functioning and treatment participation.
For individuals with COD, the impairment may be related to intellectual/cognitive ability or the mental disability. These disorders may exist in addition to the substance use disorder. The clinician should try to establish both level of intellectual/cognitive functioning in childhood and whether any impairment persists, and if so, at what level, during the periods when substance use is in full or partial remission, just as in the above discussion of diagnosis.
Determining the need for “Capable” or “Enhanced” level services
A specific tool to assess the need for “Capable” or “Enhanced” level services for persons with COD currently is not available. The consensus panel recommends a process of “practical assessment” that seeks to match the client’s assessment (mental health, substance abuse, level of impairment) to the type of services needed. The individual may even be given trial tasks or assignments to determine in concert with the counselor if her performance meets the requirements of the program being considered.
Assessment Step 8: Identify Strengths and Supports
All assessment must include some specific attention to the individual’s current strengths, skills, and supports, both in relation to general life functioning, and in relation to his or her ability to manage either mental or substance use disorders. This often provides a more positive approach to treatment engagement than does focusing exclusively on deficits that need to be corrected. This is no less true for individuals with serious mental disorders than it is for people with substance use disorders only.
Questions might focus on
- Talents and interests
- Areas of educational interest and literacy; vocational skill, interest, and ability, such as vocational skills, social skills, or capacity for creative self-expression
- Areas connected with high levels of motivation to change, for either disorder or both
- Existing supportive relationships, treatment, peer, or family, particularly ongoing mental disorder treatment relationships
- Previous mental health services and addiction treatment successes, and exploration of what worked
- Identification of current successes: What has the client done right recently, for either disorder?
- Building treatment plans and interventions based on utilizing and reinforcing strengths, and extending or supporting what has worked previously
Assessment Step 8—Application to Case Examples
Case 2. George T. had significant strengths in three areas: He had a strong desire to maintain his family, significant pride in his job, and attachment to a mutual self-help group for individuals with bipolar disorder—Manic-Depressive and Depressive Association (MDDA). Therefore his treatment plan involved attending a recovery group managed by the Employee Assistance Program (EAP) at his company (which included regularly monitored urine screens), family counseling sessions, and utilization of his weekly MDDA group for peer support. Despite not feeling engaged fully, George T. continued to attend 12-Step meetings two times per week, as there was no Dual Recovery Anonymous or Double Trouble meeting available in his area.
Case 3. Jane B. expressed significant interest in work, once her paranoia subsided. She was attempting to address her substance use on an outpatient basis, as an appropriate residential treatment program was not available. Her case management team found that she had some interest and experience in caring for animals, and, using individualized placement and support, helped her obtain a part-time job at a local pet shop two afternoons per week. She felt very proud of being able to do this, and reported that this helped her to maintain her motivation to stay away from substances and to keep taking medication.
For individuals with mental disabilities and COD, the Individualized Placement and Support model of psychiatric rehabilitation has been demonstrated to promote better vocational outcomes and (consequently) better substance abuse outcomes compared both to other models of vocational rehabilitation for this population and to outcomes when rehabilitative interventions are not offered (Becker et al. 2001). In this model, clients with disabilities who want to work may be placed in sheltered work activities based on strengths and preferences, even when actively using substances and inconsistently complying with medication regimens. In nonsheltered work activities, it is critical to remember that many employers have alcohol- and drug-free workplace policies. Participating in ongoing jobs is valuable to self-esteem in itself and can generate the motivation to address mental disorders and substance issues as they appear to interfere specifically with work success. Taking advantage of educational and volunteer opportunities also may enhance self-esteem and are often first steps in securing employment.
Social Security Disability secondary to a mental disorder, such as schizophrenia, usually is referred to as Supplemental Security Income (if the person never worked regularly), or Social Security Disability Insurance (if the person worked regularly and contributed social security payments while working). To qualify as having a mental disability, a person must have not only a confirmed major mental disorder diagnosis, but also a pattern related to the impact of that mental disorder diagnosis on his social and functional behavior that prevents employment. Social security disability benefits for an addiction disorder alone were abandoned by the Federal government in 1997. For persons with COD, disability must be caused by the mental disorder alone and not the combination of both mental and addiction disorders. Social security disability evaluation forms ask carefully about these issues and also ask whether the person is actively participating in treatments for their COD and substance abuse problems.
Assessment Step 9: Identify Cultural and Linguistic Needs and Supports
As noted above, detailed cultural assessment of individuals with substance use disorders is beyond the scope of this chapter. Cultural assessment of individuals with COD is not substantially different from cultural assessment for individuals with substance abuse or mental disorders only, but there are some specific issues that are worth addressing. These include
- Not fitting into the treatment culture (do not fit into either substance abuse or mental health treatment culture) and conflict in treatment
- Cultural and linguistic service barriers
- Problems with literacy
Not fitting into the treatment culture
To a certain degree, individuals with COD and SMI tend not to fit into existing treatment cultures. Most of these clients are aware of a variety of different attitudes and suggestions toward their disorders that can affect relationships with others. Traditional culture carriers (parents, grandparents) may have different views of their problems and the most appropriate treatment compared to peers. Individual clients may have positive or negative allegiance to a variety of peer or treatment cultures (e.g., mental health consumer movement, having mild or moderate severity mental disorders versus severe and persistent mental illness [SPMI], 12-Step or dual recovery self-help, etc.) based on past experience or on fears and concerns related to the mental disorder. Specific considerations to explore with the client include
- How are your substance abuse and mental health problems defined by your parents? Peers? Other clients?
- What do they think you should be doing to remedy these problems?
- How do you decide which suggestions to follow?
- In what kinds of treatment settings do you feel most comfortable?
- What do you think I (the counselor) should be doing to help you improve your situation?
Cultural and linguistic service barriers
Access to COD treatment is compounded by cultural or linguistic barriers. The assessment process must address specifically whether these barriers prevent access to care (e.g., the client reads or speaks only Spanish, or does not read any language) and if so, determine some possibilities for providing more individualized intervention or for integrating intervention into naturalistic culturally and linguistically appropriate human service settings.
Assessment Step 9—Application to Case Example
Case 1. Maria M. initially had difficulty identifying herself as being a victim of trauma both because she had normalized her perception of her early family experience with her abusive father and because she had received cultural reinforcement in the past that condoned the behavior of her abusive boyfriend as “normal machismo.” Referral to a group that included other Hispanic women who also had suffered abuse was very helpful to her. With the help of the group, she began to recognize the reality of the impact that trauma had had in her life.
Case 2. George T. originally was referred to Cocaine Anonymous (CA) by his counselor because the counselor knew of several local meetings with a large membership of African-American men. When George T. went, however, he reported back to the counselor that he did not feel comfortable there. First, he felt that as a family man with a responsible job he had pulled himself out of the “street culture” that was prevalent at the meeting. Second, unlike many people with COD who feel more ashamed of mental disorders than addiction, he felt more ashamed at the CA meeting than at his support group for persons with mental disorders. Therefore, for George, it was more “culturally appropriate” to refer him to 12-Step meetings attended by other middle class individuals (regardless of race) and to continue to encourage him to attend his MDDA support group for his mental disorder.
Assessment Step 10: Identify Problem Domains
Individuals with COD may have difficulties in multiple life domains (e.g., medical, legal, vocational, family, social). As noted earlier, research by McLellan and others has determined the value of providing assistance in each problem area in promoting better outcomes (McLellan et al. 1997). The ASI is a tool that is used widely to identify and quantify addiction-related problems in multiple domains, thereby determining which domains require specific attention. The value of the ASI is that it permits identification of problem domains. It is used most effectively as a component of a comprehensive assessment.
A comprehensive evaluation for individuals with COD requires clarifying how each disorder interacts with the problems in each domain, as well as identifying contingencies that might promote treatment adherence for mental health and/or substance abuse treatment. Information about others who might assist in the implementation of such contingencies (e.g., probation officers, family, friends) needs to be gathered, including appropriate releases of information.
Assessment Step 10—Application to Case Example
Case 2. Evaluation of George T. revealed several interrelated problem domains. First, it was established that work represented a major problem area, and that he risked losing his job if he did not comply with treatment. Further inquiry into the details of this expectation led the counselor to discover that the client had been evaluated by the EAP and had a very specific requirement to maintain cocaine abstinence with mandatory urine screens, meet treatment program attendance requirements, and adhere to a lithium treatment
regimen, with mandatory reports of lithium levels.
Assessment Step 11: Determine Stage of Change
A key evidence-based best practice for treatment matching of individuals with COD in both substance abuse treatment and mental health services settings is the following:
- For each disorder or problem, interventions have to be matched not only to specific diagnosis, but also to stage of change; the interventions also should be consistent with the stage of treatment for each disorder.
In substance abuse treatment settings, stage of change assessment usually involves determination of Prochaska and DiClemente Stages of Change: precontemplation, contemplation, preparation (or determination), action, maintenance, and relapse (Prochaska and DiClemente 1992). This can involve using questionnaires such as the URICA (McConnaughy et al. 1983) or the Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES) (Miller and Tonigan 1996). It also can be determined clinically by interviewing the client and evaluating the client’s responses in terms of stages of change. For example, a simple approach to identification of stage of change can be the following.
For each problem, select the statement that most closely fits the client’s view of that problem:
- No problem and/or no interest in change (Precontemplation)
- Might be a problem; might consider change (Contemplation)
- Definitely a problem; getting ready to change (Preparation)
- Actively working on changing, even if slowly (Action)
- Has achieved stability, and is trying to maintain (Maintenance)
Stage of change assessment ideally will be applied separately to each mental disorder and to each substance use disorder. For example, a client may be willing to take medication for a depressive disorder, but unwilling to discuss trauma issues (as in case 1, Maria M.); or motivated to stop cocaine, but unwilling to consider alcohol as a problem (as in case 2, George T.).
Although literature supporting the importance of stage-specific treatment has been available in both mental health and addiction literature for over a decade, very few programs routinely evaluate stage of change for the purpose of treatment matching.
In mental health settings working with individuals with SMI, the Substance Abuse Treatment Scale (SATS) (McHugo et al. 1995) is recommended strongly. This is a case-manager rated scale with eight items identified by the degree of the client’s engagement in treatment.
The stages are:
- Pre-Engagement
- Engagement
- Early Persuasion
- Late Persuasion
- Early Active Treatment
- Late Active Treatment
- Relapse Prevention
- Remission
For more in-depth discussion of the stages of change and motivational enhancement, the reader is referred to TIP 35, Enhancing Motivation for Change in Substance Abuse Treatment (CSAT 1999b).
Assessment Step 11—Application to Case Example
A 50-year-old Liberian woman with a diagnosis of paranoid schizophrenia, Lila B. illustrates the existence of differential stages of change for mental and substance abuse problems. The client permitted the case manager nurse to come to her home to give her intramuscular antipsychotic injections for her “nerves,” but would not agree to engage in any other treatment activity or acknowledge having a serious mental disorder. She also had significant alcohol dependence, with an alcohol level of 0.25 to 0.3 most of the time, with high tolerance. She denied adamantly that she had used alcohol in the last 18 months, stating that her liver was impaired and therefore unable to get rid of the alcohol. She was able to agree that she had a “mysterious alcohol level problem” that might warrant medical hospitalization for testing and perhaps treatment, as well as evaluation of her recent onset rectal bleeding.
Assessment Step 12: Plan Treatment
A major goal of the screening and assessment process is to ensure the client is matched with appropriate treatment. Acknowledging the overriding importance of this goal, this discussion of the process of clinical assessment for individuals with COD begins with a fundamental statement of principle:
- Since clients with COD are not all the same, program placements and treatment interventions should be matched individually to the needs of each client.
The ultimate purpose of the assessment process is to develop an appropriately individualized integrated treatment plan. In this model, following the work of McLellan on comprehensive services for populations with substance use disorders, Minkoff on COD, and others, the consensus panel recommends the following approach:
- Treatment planning for individuals with COD and associated problems should be designed according to the principle of mental disorder dual (or multiple) primary treatment, where each disorder or problem has a specific intervention that is matched to problem or diagnosis, as well as to stage of change and external contingencies. Figure 4-2 (p. 96) shows a sample treatment plan consisting of the problem, intervention, and goal.
- Integrated treatment planning involves helping the client to make the best possible treatment choices for each disorder and adhere to that treatment consistently. At the same time, the counselor needs to help the client adjust the recommended treatment strategies for each disorder as needed in order to take into account issues related to the other disorder.
These principles are best illustrated by using a case example to develop a sample treatment plan. For this purpose, case 2 (George T.) is used and incorporates the data gathered during the assessment process discussion above (see Figure 4-1). Note that the problem description presents a variety of information bearing on the problem, including stage of change and client strengths. Also note that no specific person is recommended to carry out the intervention proposed in the second column, since a range of professionals might carry out each intervention appropriately.
Considerations in Treatment Matching
Previous chapters introduced a variety of concepts for categorizing individuals with COD and the clinicians, programs, and systems responsible for serving those individuals. The consensus panel has identified critical factors that have been determined, either by research evidence or by consensus clinical practice, to be relevant to the process of matching individual clients to available treatment. These considerations are shown in Figure 4-3.
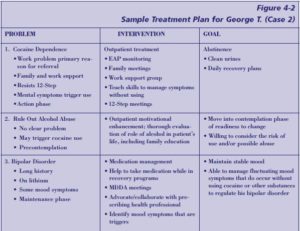


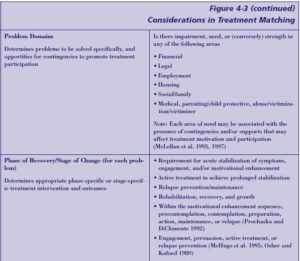
Assessment Process Summary
The assessment process described above is a systematic approach for substance abuse treatment clinicians (and mental health clinicians) to gather the information needed to develop appropriately matched treatment plans for individuals with COD. The most important question about this process, from the clinician’s standpoint, is the following:
But—can this really be done?
To answer the question, this process is approached from the perspective of a real system. Many public sector substance abuse treatment systems already define assessment procedures that require use of a level of care assessment tool (often the ASAM, but sometimes a State-derived version of the ASAM) and a comprehensive addiction severity and outcome measure (such as the ASI [McLellan et al. 1992]). How can the assessment process described here be built on these existing assessment procedures in a reasonably efficient manner?
The first steps involve engaging the client, gathering information from family and other providers, and beginning to screen for the presence of mental symptoms and disorders. The ASAM PPC-2R (and other level of care tools, such as LOCUS) will provide a reasonable way of screening for acute safety issues and presence of persistent mental disorders and disability. The ASI also provides a low-power screen for mental health difficulties (McLellan et al. 1992). These tools alone can provide a beginning picture of whether there is a need for acute mental health services intervention, ongoing case management, and/or in-depth mental assessment. The consensus panel recommends use of a low- or medium-power symptom screening tools in addition to low-power tools (e.g., M.I.N.I. or Mental Health Screening Form [Carroll and McGinley 2001]), but in many settings, ASAM plus ASI will suffice.
Next, the information gathered from ASAM and ASI can give a sufficient picture of mental impairment and substance use disorder severity to promote quadrant identification, and the ASAM itself clearly is used to identify level of care. The ASI further screens for problem domains, including a beginning picture of mental health disability.
Finally, ASAM PPC-2R includes attention to stage of change for both mental health and substance-related issues in dimension 4. Other level of care tools cover similar ground.
Through the assessment process, the counselor seeks to accomplish the following aims:
- To obtain a more detailed chronological history of past mental symptoms, diagnosis, treatment, and impairment, particularly before the onset of substance abuse, and during periods of extended abstinence.
- To obtain a more detailed description of current strengths, supports, limitations, skill deficits, and cultural barriers related to following the recommended treatment regime for any disorder or problem.
- To determine the stage of change for each problem, and identify external contingencies that might help to promote treatment adherence.
Most of these activities are already a natural component of substance abuse-only assessment; the key addition is to attend to treatment requirements and stage of change for mental disorders, and the possible interference of mental health symptoms and disabilities (including personality disorder symptoms) in addiction treatment participation.
- Confidentiality is governed by the Federal “Confidentiality of Alcohol and Drug Abuse Patient Records” regulations (42 C.F.R. Part 2) and the Federal “Standards for Privacy of Individually Identifiable Health Information” (45 C.F.R. Parts 160 and 164). ↵

